
Pregnancy Care at Maitland
Our focus for maternity care is to ensure that it is collaborative, where the woman and her family remain at the centre of the care experience and are actively involved in all decisions about the pregnancy, birth and after your baby is born. All decision making is based on relationships of mutual respect and trust.
To assist you to learn more about our services and the options of care available, please click the links below
Now that you are pregnant
Now that you are pregnant
Your care begins with your General Practitioner (GP) who will; confirm your pregnancy, taking a comprehensive healt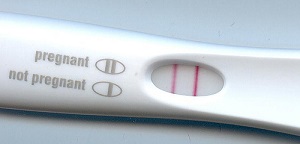 h and medical history, order your blood tests and an obstetric ultrasound.
h and medical history, order your blood tests and an obstetric ultrasound.
Your GP will write and send a referral to the Maitland Hospital antenatal clinic to initiate your care, this is usually done at around 11 -14 weeks.
Booking in visit
Once Maitland has received your completed referral, including all blood test results and scan reports, our antenatal clinic coordinator will then process your details and notify you by mail or email with an appointment time to have a booking in visit via telehealth (Phone). This visit will be attended by a midwife from our MAPS or MGP services and usually occurs around the 16th to 18th week of your pregnancy. During this visit, the midwife will discuss with you the options of care available for your pregnancy.
Where you have your pregnancy care will depend on your general health, your preferences, where you live and your previous birth experience.
Click on the image below for more information or to refer yourself to the service.
Options of care during pregnancy
Options of care during pregnancy
Midwifery Group Practice (MGP)
If you are a well healthy woman with normal risk for medical or obstetric conditions, in your first pregnancy or committed to a Vaginal birth after a caesarean (VBAC) and interested in continuity of midwifery care, this may be the model of care for you!
The MGP service offers women continuous care from booking visit with a known midwife throughout the pregnancy birth and postnatal period when you are discharged from hospital usually after 4-6 hours where the majority of postnatal care can be provided in your home. You will get to know your allocated midwife and other midwives from the team. Made up of 7 midwives, the team focuses on individualised care, early discharge from hospital and includes education and support for normal birth and breastfeeding.
Shared Care with your GP
Shared care means that you are cared for by your GP in consultation with the hospital doctors and midwives. You will need to come to the Antenatal Clinic at Maitland for a Booking-in visit, and a second visit usually around 36 weeks. Shared Care enables you to continue seeing your family doctor, who you already know and trust, during your pregnancy, and this may be more convenient for you.
Midwifery Antenatal and Postnatal Service (MAPS)
Under the MAPS model of care, you will have been allocated to a small team of midwives who were responsible for providing you with antenatal care during your pregnancy. This same team will continue to provide care for you and your newborn in the comfort of your own home environment after you are discharged from hospital.
Women who are considered to be low risk will be encouraged to be discharged home from birthing suite following the birth of their baby. This may be as soon as 4 hours following birth.
If you require a longer stay in hospital you will be transferred to the maternity ward. When you are discharged from hospital following the birth of your baby, please phone your midwife to notify her of your birth and discharge.
Your MAPS midwifery team will work with you to provide close follow-up care and support in your own home after the birth of your baby. Below is the schedule of home visits following discharge. If you have a longer stay in hospital this schedule will be adjusted accordingly. Also if a higher level of postnatal care is required your midwife will work with you to determine an appropriate schedule.
Your MAPS midwife will:
- visit you in the comfort of your own home giving you one-to-one advice and support
- support you with feeding your baby
- advise you on helping your baby to sleep
- support with caring for your baby, eg: bathing
- weigh your baby
- perform the routine newborn bloodspot screening test if required
- complete your postnatal check
- provide you with support and reassurance
- put you in contact with the Child and Family Health Nursing Service.
you may choose to use this service directly from the Birth Suite or within a couple of days of having your baby
Day 1 | Discharge home from birthing suite after birth. Phone call from your midwife in the afternoon. |
Day 2 or 3 | Your midwife will provide a home visit on either day 2 or day 3. Your midwife will work with you to determine what is most appropriate for you and your baby. |
Day 5 | Postnatal home visit and discharge from service if appropriate. |
Specialist Obstetric Care at Maitland Antenatal Clinic
Specialist Obstetricians are best able to care for women who have complications in pregnancy such as:
- Had a previous pregnancy requiring specialist care and/or hospitalisation
- A pregnancy that is not progressing normally
- A multiple pregnancy, e.g. twins
- Diabetes and/or other medical complications
Consultation with an Obstetrician may be required at any point in your pregnancy if there are any changes required to your chosen model of care
Care with a Private Obstetrician
Women seeing a private obstetrician may birth at the Maitland Hospital. Women choosing this option of care will see their obstetrician for all their antenatal care in their obstetrician’s private consulting rooms. It is important if you choose this care option that you attend an administrative booking visit at the Maitland Admissions Office at around 24 weeks pregnant.
Aboriginal Maternal Health Service
Naae-Wanni provides care for Aboriginal and Torres Strait Islander women, and/or women whose baby will identify as Aboriginal and/or Torres Strait Islander. The Naae-Wanni service aims to provide support and education during pregnancy, and after birth in a culturally safe environment. The service endeavours to offer holistic care which includes the woman, her baby, partner, family and community. This service includes antenatal care, support service referrals and health education, also working closely with other Aboriginal services within the community.
You may contact the staff at Naae-Wanni directly or talk to your GP or the staff at the antenatal clinic to make a referral to our service. Please contact: 0400333884
Next Birth after Caesarean
For pregnant women who have experienced a caesarean section for a previous birth, they may be considering the best birth option for their current pregnancy. At The Maitland hospital, we acknowledge that a vaginal birth after a previous caesarean section is often a suitable and safe option for the majority of women. Your midwife will discuss this with you at your first booking visit.
At The Maitland Hospital, we offer free education sessions to help the woman and her partner to further explore their birth options and assist their decision making. In these education sessions the woman will also discover strategies to optimise the birth experience regardless of her birth intention.
Summary of options of care available
| Options of care | Suitability | Who will provide your antenatal care | Where you will have your antenatal care | Where you will have your baby |
|---|---|---|---|---|
| Midwifery Group Practice (MGP) | Women with uncomplicated pregnancy | Known midwife from the MGP | Antenatal Clinic | Maitland Birth Suite |
| Shared Care with GP | Women with uncomplicated pregnancy | GP of your choice; Antenatal Clinic midwife at Booking-in and 36 weeks | GP practice; 1 visit prior to 20 weeks and 2nd visit at Maitland Antenatal clinic | Maitland Birth Suite |
| Midwifery Care in Community Antenatal Clinics | Women with uncomplicated pregnancy | Midwives from Maitland MAPS Team | Antenatal Clinic | Maitland Birth Suite |
| Naae-Wanni/AMIHS Service | Aboriginal and Torres Strait Island women or women having an Aboriginal and Torres Strait Island baby | Naae-Wanni midwives and Aboriginal Health Care Workers | Community Antenatal Clinics/ Mindaribba | Maitland Birth Suite |
| Care with private Obstetrician | All women | Private Obstetrician | Private rooms | Maitland Birth Suite |
| Specialist Care at Maitland Hospital | Women with pregnancies complicated by medical, obstetric conditions | Medical Obstetric teams | Maitland Antenatal Clinic | Maitland Birth Suite |
Pregnancy support services
Pregnancy support services
Early Pregnancy Assessment Service
This service is available for women with early pregnancy abdominal pain, bleeding or severe vomiting (up to 18 weeks).
A referral by a medical practitioner (General Practice or Emergency Department) is required for this service. There is no capacity for self-referral.
Multicultural Health Services
The Multicultural Health Unit provides the following services to women from culturally and linguistically diverse (CALD) backgrounds:
Health Care Interpreter Services
The Multicultural Health Unit provides professional health care interpreters for all women from CALD backgrounds. Health Care Interpreters assist women to communicate with their health professional during antenatal visits, classes, labour, postnatal period and other health-related occasions. If you need the assistance of a health care interpreter, please let staff know and they will arrange this for you.
Aboriginal Hospital Liaison Officers
The Maitland Hospital Aboriginal Hospital Liaison Officer is available to assist Aboriginal and Torres Strait Islander patients.
If you or your family require assistance in accessing hospital services, please ask one of our staff members to contact the Aboriginal Liaison Officer for you.
Care and Support for women with drug and alcohol problems
Some women may still be using alcohol or taking drugs during pregnancy. Alcohol and drugs can have harmful effects on unborn babies. Our staff can offer a range of support for you to optimise your health and the health of your unborn baby.
Providing practical assistance and counselling: Social Work
Social workers are part of the health care team looking after you and your family while you are in hospital. In some situations, the social worker will routinely come to see you during your stay or at the time of your antenatal appointment. You may also wish to contact them yourself. This service is confidential and free.
Social Workers can offer counselling to individuals and families in all areas, including:
- Women or families experiencing difficulties during the pregnancy, such as family breakdown or financial difficulties
- Women or families considering adoption
- Information about community support services
If you wish to contact a social worker, you can contact the Social Work Department directly on (02) 4939 2628 or ask your midwife, doctor or other hospital staff involved in your care to contact a social worker for you.
Promoting Healthy Eating
Both you and your baby need extra nutrients during all stages of pregnancy and breastfeeding. Eating a nutritious diet during pregnancy promotes healthy growth and development for your baby, prepares you for breastfeeding and is important for your own wellbeing. It is important to remember that even though you are eating for two, there is no need to eat twice as much.
A dietitian can assess your diet and suggest any changes that you may need to make. This is particularly important for women who are under- or over-weight, suffer from anaemia or a malabsorption illness such as Crohn’s or Coeliac disease or you follow a vegetarian diet.
If you develop diabetes in your pregnancy you will be referred to the Hunter Diabetes Service who have dedicated dieticians and a diabetic educator to assist you with meal plans and blood sugar control.
Whilst you are in hospital, dietetics can also provide nutrition advice or organise meal plans/ menus for you if you require therapeutic diets.
If you need to arrange to see the dietitian in your pregnancy your midwife or doctor can refer you.
Get Healthy in Pregnancy
The Get Healthy in Pregnancy Service is a FREE telephone health coaching service available to anyone aged 16 years and over. You will be able to talk with a qualified dietitian or exercise physiologist over the phone in the privacy of your own home.
Your health coach could help you to:
- Eat healthily
- Get active
- Gain or maintain a healthy amount of weight during your pregnancy
- Not drink alcohol during your pregnancy
- Return to your pre-pregnancy weight.
For Aboriginal women or women carrying an Aboriginal baby you may be able to speak with the Get Healthy Aboriginal Liaison Officer, for your first phone call or one of your coaching calls. The ALO will talk to you about your needs and your access to services in the community before referring you to either a dietitian or an exercise physiologist for the remainder of your phone calls.
Discuss referral to the service with your midwife at your booking-in visit or you can click the image below for more information and to refer yourself to the service.
Helping women to move well: Physiotherapy
A physiotherapist is available to give you advice or treatment on the discomforts that may arise during your pregnancy or after your baby is born. These may include back pain, pelvic pain, pelvic floor weakness, incontinence or abdominal muscle weakness.
If you wish to see a physiotherapist, you may ask your caregiver (midwife or Doctor) to refer you to the Physiotherapy department.
Get Healthy in Pregnancy
The Get Healthy in Pregnancy Service is a FREE telephone health coaching service available to anyone aged 16 years and over. You will be able to talk with a qualified dietitian or exercise physiologist over the phone in the privacy of your own home.
Your health coach could help you to:
- Eat healthily
- Get active
- Gain or maintain a healthy amount of weight during your pregnancy
- Not drink alcohol during your pregnancy
- Return to your pre-pregnancy weight.
For Aboriginal women or women carrying an Aboriginal baby you may be able to speak with the Get Healthy Aboriginal Liaison Officer, for your first phone call or one of your coaching calls. The ALO will talk to you about your needs and your access to services in the community before referring you to either a dietitian or an exercise physiologist for the remainder of your phone calls.
Discuss referral to the service with your midwife at your booking-in visit or you can
Click the image below for more information and to refer yourself to the service.
Maitland Birth Suite
Birth suite
The Maitland Hospital Birth Suite is located on the first floor, access is through the lifts past information on ground floor.
When you arrive at the hospital, go straight to the Birth Suite reception desk where you will be met by a midwife and taken to an available room. This unit is locked you will need to press the buzzer to gain access to the unit.
Maternity Assessment Day Unit (Daystay)
The MADU is an area where pregnant women may be directed to go following an antenatal clinic visit or after speaking with a midwife in Birth Suite. Reasons may include: being more than 41 weeks pregnant, waters leaking after 37 weeks and not in labour, high blood pressure, and other events. While in MADU, a comprehensive assessment will be undertaken, and this could take about 4 hours. When you are ready to birth or require closer monitoring, you will be transferred to the birth suite. Alternatively, you may be discharged home from MADU with a follow up plan of care.
Travelling to have your baby in hospital
- Contact the midwife in the Birth Suite (or your own midwife as arranged) for advice.
- Wear a sanitary pad (or more!).
- Have your support person drive safely and use your seat belt with lap belt positioned below your baby. Have old towels available to catch leaks if they occur, and an old ice-cream bucket in case of nausea or vomiting.
In NSW, an ambulance ride can be very expensive; it is strongly suggested that you join an ambulance fund for your family emergency situations, if you are not already covered by private health insurance (this may be done through any major private health fund office or online).
Bring your antenatal record. Your antenatal record provides us with your history and plan of management for labour and birth. Please carry it at all times and present it to the midwife or receptionist on your arrival to the Birth Suite.
Going home from the Birth Suite
For most women, pregnancy and birth is a healthy experience. Some women may even choose to go home straight from the Birth Suite a few hours after their baby is born. This may be an option for you if you have good family support, you and your baby are well and your baby has had his/her first feed. A physical examination of you both will be attended before you leave. All the necessary documents and supportive information will also be provided. Midwives working on the MAPS teams usually offer daily postnatal home visits for about 5 days after birth dependant on your circumstances. The MGP service is up to 6 weeks after birth.
Chosen support person for birth
At Maitland Hospital we encourage you to have the support person of your choice with you in labour. Women who are well supported in labour use less medical pain relief which can delay the establishment of breastfeeding.
Comfort measures for labour
There are many things you can do to make labour easier. Non-medical comfort measures can help to avoid medication in labour which may make it harder to establish breastfeeding. Staying active and moving in labour makes contractions more effective and can add to your comfort as can warm showers, warm packs, relaxing, position changes, music and any distraction techniques.
Doulas
It is the woman’s choice who supports her during pregnancy, labour, birth and the postnatal period. A doula is a layperson, identified by the woman, who provides continuous support during the antenatal period, childbirth and the postnatal period. The doula attends as an employee of the woman. Under normal circumstances each woman is able to have two support people with her in the Birth Suite. A doula is to be considered one of the two support people.
Hunter New England Local Health District (HNELHD) is open to the use of doulas at birth, and maternity services will facilitate a productive, receptive environment for doulas to support women. However, HNELHD clearly states that it does not accept responsibility and is not accountable for any actions or advice given to labouring women by doulas.
Visitors
If there are some visitors you would like to visit you soon after the birth of your baby in the Maitland Birth Suite, we request that your visitors check at the Maitland Birth Suite desk before proceeding to your room. This is to protect your privacy and the privacy of other women in the unit.
Enquiries while in the Birth Suite
To protect your privacy and confidentiality, information is not given to people enquiring about you without your consent. Encourage your family to contact your support person for any information.
Video recording and photography
We respect your wish to film labour and birth. However, all staff have the right to refuse to be identified on film or refuse filming during specific procedures. Please inform your midwife of your intention to film. If your baby is born in the Operating Suite, only still photographs may be taken.
Children
There are no childcare facilities at Maitland Hospital. If you wish to have your children present for labour and birth, we request you have one adult, other than your main support person to care and supervise. However, the limit of two additional people at a time will also need to be considered.
Mobile phones
We ask that all mobile phones are turned to silent mode in the Birth Suite and ward environments.
Keeping baby with you following birth
Your baby will remain with you following birth. Skin-to-skin is encouraged for a minimum of 1 hour after the birth or until the first breastfeed. Skin to skin contact stimulates the mothers’ production of the oxytocin hormone, which decreases bleeding, promotes bonding and breastfeeding. It allows the baby to smell, touch and know mum as well as stay warm. When the baby shows signs of readiness, they will be able to breastfeed.
It is strongly suggested that during this important time the baby stays with mum, rather than being handed around to other family members. The father of the baby has an important role in protecting the new mother and baby.
After your baby has fed, they will be weighed and measured. With your consent, Vitamin K (Konakion) and Hepatitis B vaccine injections will be given at this time.
Two arm-bands with the baby’s correct identification details will be placed on both the baby’s legs – the midwife will ask you to check these details to ensure they are accurate. The arm bands will state baby of Mothers name, date of birth and babies date of birth. Sometimes handwritten arm bands will be used until, baby’s official labels are printed.
The armbands are routinely checked by the midwives. Should the armbands fall off, please tell the midwife as soon as you can so that new armbands can be provided.
If medical treatment is required for your baby, then they may be taken to the Special Care Nursery adjacent to the Birth Suite. As soon as possible, you will be able to visit and care for your baby. Depending on your baby’s medical condition skin to skin contact with your baby will be encouraged.
What happens to the placenta (afterbirth)?
After the birth of your baby, the placenta will be disposed of in accordance with NSW Health Guidelines.
On some occasions the placenta may be sent to the Pathology Department for further testing, to provide extra information. This may happen if you gave birth to twins, or if you or your baby has a serious medical or obstetric condition.
If you would like to take your placenta home, please talk to your midwife.
Stem cell collection and storage
If you are interested in the collection of stem cells from your baby’s cord blood for possible future use, you need to organise this with one of the private companies several weeks before coming to hospital to birth your baby. You will need to organise the collection, equipment, courier service and storage with the private company.

