
Pregnancy Care at Tamworth
Our focus for maternity care is to ensure that it is collaborative, where the woman and her family remain at the centre of the care experience and are actively involved in all decisions about the pregnancy, birth and after your baby is born. All decision making is based on relationships of mutual respect and trust.
To assist you to learn more about our services and the options of care available, please click the links below
Now that you are pregnant
Now that you are pregnant
Your care begins with your General Practitioner (GP), by confirming your pregnancy, taking a comprehensive health and medical history, ordering your blood tests and an obstetric ultrasound.
You should see your GP around 8 weeks pregnant and they will write and send a referral to the Tamworth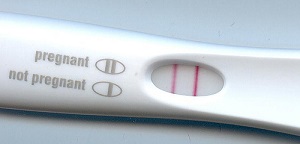 Hospital antenatal clinic to initiate your care.
Hospital antenatal clinic to initiate your care.
Once we have received your completed referral, including all blood test results and scan reports, our antenatal clinic coordinator will then process your details and notify you by mail with an appointment time to have a booking in visit. This visit will be attended by a midwife at Tamworth Hospital and usually occurs between 11 - 14 weeks. During this visit, the midwife will discuss with you the options of care available for your pregnancy.
Where you have your pregnancy care will depend on your general health, your preferences, where you live and your previous birth experience.
You will also be scheduled for an obstetric visit between 16-22 weeks, depending on the referral from your GP and the information provided at your booking in visit. Our obstetricians will confirm your agreed model of care during your pregnancy.
The midwife will also discuss the importance of healthy eating and physical activity during this visit. You will be offered a referral to the Get Healthy in Pregnancy service. The Service is open to anyone aged 16 years and over. You will be able to talk with a qualified dietitian or exercise physiologist over the phone in the privacy of your own home. For Aboriginal women or women carrying an Aboriginal baby you may be able to speak with the Get Healthy Aboriginal Liaison Officer (ALO), for your first phone call or one of your coaching calls. The ALO will talk to you about your needs and your access to services in the community before referring you to either a dietitian or an exercise physiologist for the remainder of your phone calls.
Click on the image below for more information or to refer yourself to the service.
Options of care during pregnancy
Options of care during pregnancy - Tamworth
Shared Care with your GP
This care model provides the option of seeing either your own GP or a midwife at your GP practice for appointments during pregnancy, as well as attending appointments at the hospital Antenatal Clinic. If there are no complications with your pregnancy, and your GP offers a Shared Care service with GP or GP Practice Midwife, your GP or GP Practice Midwife can provide most of your antenatal care from their practice. You will visit the hospital Antenatal Clinic early in your pregnancy at 16-18 weeks, again at 28 weeks and from 36 weeks as agreed with the hospital Obstetric team. Your baby will be born at Tamworth
Hospital. If any complications arise during your pregnancy, your GP will refer you to the Maternity Obstetric team.
Midwifery Care (Hospital based/ Coledale community centre/ Tamworth Aboriginal Medical Service)
Following an initial antenatal clinic visit with an obstetrician, you have the option of choosing midwifery care at our Antenatal Clinic if you are generally well and having an uncomplicated pregnancy. The Antenatal Clinic's midwives will care for you during your clinic visits. If you develop complications during the course of your pregnancy, you may be referred into the care of the Maternity Obstetric team for some or all of your future appointments.
Specialist Obstetric Care at TRRH Antenatal Clinic
If you experience complications during your pregnancy, you will be referred under the care of one of our obstetricians or registrars in the Maternity Obstetric team at the hospital Antenatal Clinic. Specialist Obstetricians are best able to care for women who have pregnancies complicated by:
- A previous pregnancy requiring specialist care and/or hospitalisation
- pregnancy that is not progressing normally
- A multiple pregnancy, e.g. twins
- Diabetes and/or other conditions
Care with a Private Obstetrician
Full obstetric care is available privately through obstetricians’ offices. Your booking-in appointment at the Antenatal Clinic may be later in your pregnancy, at 20-28 weeks, and you will not need a visit with the Maternity Obstetric team. Your baby will be born at Tamworth Hospital.
Tamworth Aboriginal Mothers and Babies Service (AMBS)
 The AMBS provides care for Aboriginal and Torres Strait Islander women, and/or women whose baby will be Aboriginal and Torres Strait Islander. The service aims to provide culturally appropriate support and education during pregnancy, after birth and for children up to early school years. This service includes antenatal and postnatal care, support service referrals and health education. You may contact the staff directly, or talk to your GP or the staff at the antenatal clinic to make a referral to the AMBS service.
The AMBS provides care for Aboriginal and Torres Strait Islander women, and/or women whose baby will be Aboriginal and Torres Strait Islander. The service aims to provide culturally appropriate support and education during pregnancy, after birth and for children up to early school years. This service includes antenatal and postnatal care, support service referrals and health education. You may contact the staff directly, or talk to your GP or the staff at the antenatal clinic to make a referral to the AMBS service.
Clinics are also available:
- Thursdays at Coledale Community Centre between 10am and 3pm, or
- Fridays at the Tamworth Aboriginal Medical Centre between 10am and 3pm.
Other times can be arranged by contacting the service on 0408 699 624.
Summary of models of care available
Summary of models of care available
| Options of Care | Suitability | Who will provide your antenatal care | Where you will have your baby | Who will provide care during labour and birth |
|---|---|---|---|---|
| Tamworth Midwifery Group Practice (TMGP) | Women with uncomplicated pregnancy | Known midwife from the TMGP | Home/Antenatal Clinic | Known midwife from the TMGP |
| Midwifery Care Antenatal Clinic Tamworth Hospital | Women with uncomplicated pregnancy | Midwives from Tamworth Hospital | Antenatal Clinic Tamworth Hospital | Midwife from Maternity Unit |
| Shared Care with GP | Women with uncomplicated pregnancy | GP of your choice; Antenatal Clinic midwife at Booking-in and 36 weeks | GP Practice and Antenatal Clinic | Midwife from Maternity Unit |
| Tamworth Aboriginal Mothers and Babies Service (AMBS) | Aboriginal and Torres Strait Island women or women having an Aboriginal and Torres Strait Island baby | Midwives and Aboriginal Health Care Workers | Home / Community AMBS Clinics | Midwife from Maternity Unit |
| Care with private Obstetrician | All women | Private obstetrician | Private rooms | Midwife from Maternity Unit |
| Specialist Care at Tamworth Hospital | Women with pregnancies complicated by medical, obstetric conditions | Medical Obstetric teams and Midwives from Tamworth Hospital | Tamworth Antenatal Clinic | Midwife from Maternity Unit |
WYSIWYG Content Container |
Pregnancy support services
Pregnancy support services - Tamworth
Early Pregnancy Assessment Service (EPAS)
This service is available for women with early pregnancy abdominal pain, bleeding or severe vomiting (up to 18 weeks).
A referral by a medical practitioner (General Practice or Emergency Department) is required for this service. There is no capacity for self-referral.
Multicultural Health Services
The Multicultural Health Unit provides the following services to women from culturally and linguistically diverse (CALD) backgrounds:
Health Care Interpreter Services
The Multicultural Health Unit provides professional health care interpreters for all women from CALD backgrounds. Health Care Interpreters assist women to communicate with their health professional during antenatal visits, classes, labour, postnatal period and other health-related occasions. If you need the assistance of a health care interpreter please let staff know and they will book one for your appointment.
Aboriginal Liaison Officers
The Tamworth Hospital Aboriginal Liaison Officer is available to assist Aboriginal and Torres Strait Islander patients and is available each Tuesday.
Care and Support for women with drug and alcohol problems
Some women may still be using alcohol or taking drugs during pregnancy. It is known that this can be very harmful to the unborn child. A number of skilled, non-judgmental and empathetic staff can provide a range of support. This will greatly improve the chances of having a healthy baby. Other services include the Drug and Alcohol Team and Social Work team.
Providing practical assistance and counselling: Social Work
Social workers are part of the health care team looking after you and your family while you are in hospital. In some situations, the social worker will routinely come to see you during your stay or at the time of your antenatal appointment. This service is confidential and free.
Social Workers can offer counselling to individuals and families in all areas, including:
- Women or families experiencing difficulties during the pregnancy, such as family breakdown or financial difficulties
- Women or families considering adoption
- Information about community support services
If you wish to contact a social worker, ask your midwife, doctor or other hospital staff involved in your care to contact a social worker for you.
Promoting Healthy Eating: Dietitians
Both you and your baby need extra nutrients during all stages of pregnancy and breastfeeding. Eating a nutritious diet during pregnancy promotes healthy growth and development for your baby, prepares you for breastfeeding and is important for your own wellbeing. It is important to remember that even though you are eating for two, there is no need to eat twice as much.
A dietitian can assess your diet and suggest any changes that you may need to make. This is particularly important for women who are under- or over-weight, suffer from anaemia or a malabsorption illness such as Crohn’s or Coeliac disease, follow a vegetarian diet, or are diabetic.
If you wish to see a dietitian, ask your midwife, doctor or other hospital staff involved in your care to contact a dietitian for you.
Get Healthy in Pregnancy
The Get Healthy in Pregnancy Service is a FREE telephone health coaching service available to anyone aged 16 years and over. You will be able to talk with a qualified dietitian or exercise physiologist over the phone in the privacy of your own home.
Your health coach could help you to:
- Eat healthily
- Get active
- Gain or maintain a healthy amount of weight during your pregnancy
- Not drink alcohol during your pregnancy
- Return to your pre-pregnancy weight.
For Aboriginal women or women carrying an Aboriginal baby you may be able to speak with the Get Healthy Aboriginal Liaison Officer, for your first phone call or one of your coaching calls. The ALO will talk to you about your needs and your access to services in the community before referring you to either a dietitian or an exercise physiologist for the remainder of your phone calls.
Discuss referral to the service with your midwife at your booking-in visit or you can click the image below for more information and to refer yourself to the service.
This service can be accessed online or discuss referral with the midwife at your booking in visit.
Helping women to move well: Physiotherapy
A physiotherapist is available to give you advice or treatment on the discomforts that may arise during your pregnancy or after your baby is born. These may include back pain, pelvic pain, pelvic floor weakness, incontinence or abdominal muscle weakness.
If you wish to see a physiotherapist, ask your midwife, doctor or other hospital staff involved in your care to contact a physiotherapist for you.
Tamworth Birth Suite
Birthing suite and Birth Centre - Tamworth
The Tamworth Birth Suite is located on Level 3 of the Acute Service Building.
When you arrive at Birth Suite, you will be met by a midwife or receptionist.
Travelling to have your baby in hospital
- Contact the midwife in the Birthing Service (or your own midwife as arranged) for advice.
- Wear a sanitary pad(or more!).
- Have your support person drive safely, and use your seat belt with lap belt positioned below your baby. Have old towels available to catch leaks if they occur, and an old ice-cream bucket in case of nausea or vomiting.
- In NSW, an ambulance ride can be very expensive; it is strongly suggested that you join an ambulance fund for your family emergency situations, if you are not already covered by private health insurance (this may be done through any major private health fund office or online).
- Bring your antenatal record. Your antenatal record provides us with your history and plan of management for labour and birth. Please carry it at all times, and present it to the midwife on your arrival to the Birth Suite.
A plan for going home after birth
For most women, pregnancy and birth is a healthy experience. Many women choose to go home from the hospital soon after the baby is born, and take advantage of our Home Midwifery Service (HMS). This is dependent on both mother and baby being well, baby has had the first feed, and mother is confident going home with adequate family support. You can go home straight from Birth Suite 4-6 hours after birth. A physical examination of mother and baby will be done before you leave. All the necessary documents and supportive information will also be provided. The midwife from the HMS or Midwifery Group Practice will contact you the day after your birth and inform you of an approximate time for your home visit. They may visit you for up to about 5 days after birth, depending on your circumstances.
Husband/ partner/ support persons in labour and birth
We welcome people who will support and encourage you throughout labour and birth. There is room for a maximum of two support people at any one time in the Birth Suite.
Doulas
It is the woman's choice who supports her during pregnancy, labour, birth and the postnatal period. A doula is a layperson, identified by the woman, who provides continuous support during the antenatal period, childbirth and the postnatal period. The doula attends as an employee of the woman. Under normal circumstances each woman is able to have two support people with her in delivery suite. A doula is to be considered one of the two support people.
Hunter New England Local Health District (HNELHD) is open to the use of doulas at birth, and maternity services will facilitate a productive, receptive environment for doulas to support women. However, HNELHD clearly states that it does not accept responsibility and is not accountable for any actions or advice given to labouring women by doulas.
Visitors
If there are visitors you would like to visit you soon after the birth of your baby in the Birth Suite, we request that your visitors check at the Birth Suite desk before proceeding to your room. This is to protect your privacy and the privacy of other women in the unit.
Enquiries while in Birth Suite
To protect your privacy and confidentiality, information is not given to people enquiring about you without your consent. We will take messages for you to contact the enquirers at a convenient time.
Video recording and photography
We respect your wish to film labour and birth. However, all staff have the right to refuse to be identified on film or refuse filming during specific procedures. Please inform your midwife of your intention to film. If your baby is born in the Obstetric Operating Suite, only still photographs may be taken.
Children
There are no childcare facilities available in the maternity unit. If you wish to have your children present for labour and birth, we request you have one adult, other than your main support person to care and supervise. However, the limit of two additional people at a time will also need to be considered.
Mobile phones
We ask that all mobile phones are turned to silent mode in the Birth Suite, and ward environments.
Keeping baby with you following birth
Your baby will remain with you following birth. Skin-to-skin is encouraged for a minimum of 1 hour after the birth or until the first breastfeed. Skin to skin contact stimulates the mothers' production of the oxytocin hormone, which decreases bleeding, promotes bonding and breastfeeding. It allows the baby to smell, touch and know mum as well as stay warm. When the baby shows signs of readiness, he/she will be able to breastfeed.
It is strongly suggested that during this important time the baby stays with mum, rather than being handed around to other family members. The father of the baby has an important role in protecting the new mother and baby.
After your baby has fed, he / she will be weighed and measured. With your consent, Vitamin K (Konakion) and Hepatitis B vaccine injections will be given at this time.
Two arm-bands with the baby's correct identification details will be placed on the baby's arm and leg – the midwife will ask you to check these details to ensure they are accurate. The armbands are routinely checked by the midwives. Should the armbands fall off, please tell the midwife as soon as you can so that new armbands can be provided.
If medical treatment is required for your baby, then he or she may be taken to the Special Care Nursery adjacent to the Birth Suite. As soon as possible, you will be able to visit and care for your baby.
What happens to the placenta (afterbirth)?
After the birth of your baby, the placenta will be disposed of in accordance with NSW Health Guidelines.
On some occasions the placenta may be sent to the Pathology Department, for extra information. This may happen if you gave birth to twins, or if you or your baby has a serious medical or obstetric condition. If you would like to take your placenta home please talk to your midwife.
Stem cell collection and storage
If you are interested in the collection of stem cells from your baby's cord blood for possible future use, you need to organise this with one of the private companies several weeks before coming to hospital to birth your baby. You will need to organise the collection, equipment, courier service and storage with the private company.

