Maternity Services at Gunnedah Hospital
Congratulations on your pregnancy and welcome to the Gunnedah Hospital Birthing Service.
The Gunnedah Hospital provides maternity care to women who live in Gunnedah area, and other women and babies transferred for care from across the Hunter New England Local Health District and other parts of NSW.
Our team care for healthy women and their babies greater than 37 weeks gestation, as well as those with a wide range of more complicated needs. Our aim is to provide what we call ‘women-centred care.’ This means that we want to work with you to tailor your care to meet your individual needs.
The Gunnedah Hospital has been caring for women and babies since it opened its doors in 1964. Around 160 babies are born at Gunnedah Hospital each year.
Our Maternity team in Gunnedah, including our local GP Obstetricians will provide pregnancy and labour care to all women with uncomplicated pregnancies who have their babies after 37 weeks pregnant. If you pregnancy is complicated or you need to have your baby early we will discuss with you the need to transfer to a larger District or John Hunter Hospital.
Our team are also committed to ensuring that you have a safe and positive birth experience and that you have the support you need to begin caring for your newborn baby.
Please click here to learn more about your Rights and Responsibilities as a patient, carer or community member of the Hunter New England Local Health District
Yours Sincerely,
Therese Mills
Midwife Unit Manager
Download the NSW Health Having a Baby Book here
Gunnedah Maternity Telephone Numbers: | |
| Maternity Unit | 02 67418037 |
| Birth & Parenting programs (Parenting Education Service) | 02 67418037 |
| Aboriginal Maternal Infant Health Service | 02 67418000 |
Pregnancy Care at Gunnedah
Now that you are pregnant
Now that you are pregnant
 Your care begins with your General Practitioner (GP), by confirming your pregnancy, taking a comprehensive health and medical history, ordering your blood tests and an obstetric ultrasound.
Your care begins with your General Practitioner (GP), by confirming your pregnancy, taking a comprehensive health and medical history, ordering your blood tests and an obstetric ultrasound.
Your GP will write and send a referral to the Gunnedah Hospital Maternity Ward to initiate your care.
Once we have received your completed referral, including all blood test results and scan reports, you will then need to ring admissions to arrange an appointment time to have a booking- in visit. This visit will be attended by a midwife at Gunnedah Maternity Unit. You will need to make a booking in appointment with the hospital midwives for between 11-14 weeks gestation.
Where you have your pregnancy care will depend on your general health, your preferences, where you live and your previous birth experience. You will then have the option to have an antenatal visit with the midwives at the hospital at 28 weeks and 36 weeks gestation.
The midwife will also discuss the importance of healthy eating and physical activity during this visit. You will be offered a referral to the Get Healthy in Pregnancy service. The Service is open to anyone aged 16 years and over. You will be able to talk with a qualified dietitian or exercise physiologist over the phone in the privacy of your own home. For Aboriginal women or women carrying an Aboriginal baby you may be able to speak with the Get Healthy Aboriginal Liaison Officer (ALO), for your first phone call or one of your coaching calls. The ALO will talk to you about your needs and your access to services in the community before referring you to either a dietitian or an exercise physiologist for the remainder of your phone calls.
Click on the image below for more information or to refer yourself to the service.
Gunnedah Birth suite
Gunnedah Birth Suite
The Gunnedah Hospital Birth Suite is located within the Maternity Unit.
When you arrive at Gunnedah Hospital after hours, you will need to enter through the Emergency Department unless other arrangements have been made with the midwife.
Travelling to have your baby in hospital
- Contact the midwife in the Birthing Service (or your own midwife as arranged) for advice.
- Have your support person drive safely, and use your seat belt with lap belt positioned below your baby. Have old towels available to catch leaks if they occur, and an old ice-cream bucket in case of nausea or vomiting.
- In NSW, an ambulance ride can be very expensive; it is strongly suggested that you join an ambulance fund for your family emergency situations, if you are not already covered by private health insurance (this may be done through any major private health fund office or online).
- Bring your antenatal record. Your antenatal record provides us with your history and plan of management for labour and birth. Please carry it at all times, and present it to the midwife on your arrival.
Husband/ partner/ support persons in labour and birth
We welcome people who will support and encourage you throughout labour and birth. There is room for a maximum of two support people at any one time in the Birth Suite, COVID restrictions permitting.
Doulas
It is the woman’s choice who supports her during pregnancy, labour, birth and the postnatal period. A doula is a layperson, identified by the woman, who provides continuous support during the antenatal period, childbirth and the postnatal period. The doula attends as an employee of the woman. Under normal circumstances each woman is able to have two support people with her in delivery suite. A doula is to be considered one of the two support people.
Hunter New England Local Health District (HNELHD) is open to the use of doulas at birth, and maternity services will facilitate a productive, receptive environment for doulas to support women. However, HNELHD clearly states that it does not accept responsibility and is not accountable for any actions or advice given to labouring women by doulas.
Visitors
If there are some visitors you would like to visit you soon after the birth of your baby in the Maternity unit, we request that your visitors check at the Maternity Unit desk before proceeding to your room. This is to protect your privacy and the privacy of other women in the unit.
Enquiries while in Birth Suite
To protect your privacy and confidentiality, information is not given to people enquiring about you without your consent. We will take messages for you to contact the enquirers at a convenient time.
Video recording and photography
We respect your wish to film labour and birth. However, all staff have the right to refuse to be identified on film or refuse filming during specific procedures. Please inform your midwife of your intention to film.
Children
There are no childcare facilities available in the maternity unit. If you wish to have your children present for labour and birth, we request you have one adult, other than your main support person to care and supervise. However, the limit of two additional people at a time will also need to be considered.
Mobile phones
We ask that all mobile phones are turned to silent mode in the Birth Suite, and ward environments.
Keeping baby with you following birth
Your baby will remain with you following birth. Skin-to-skin is encouraged for a minimum of 1 hour after the birth or until the first breastfeed. Skin to skin contact stimulates the mothers’ production of the oxytocin hormone, which decreases bleeding, promotes bonding and breastfeeding. It allows the baby to smell, touch and know mum as well as stay warm. When the baby shows signs of readiness, he/she will be able to breastfeed.
It is strongly suggested that during this important time the baby stays with mum, rather than being handed around to other family members. The father of the baby has an important role in protecting the new mother and baby.
After your baby has fed, he / she will be weighed and measured. With your consent, Vitamin K (Konakion) and Hepatitis B vaccine injections will be given at this time.
Two arm-bands with the baby’s correct identification details will be placed on the baby’s arm – the midwife will ask you to check these details to ensure they are accurate. The identifying number on the mother’s armbands are the same as the baby’s, so it is important that you make sure the identifying numbers correspond.
The armbands are routinely checked by the midwives. Should the armbands fall off, please tell the midwife as soon as you can so that new armbands can be provided.
What happens to the placenta (afterbirth)?
After the birth of your baby, the placenta will be disposed of in accordance with NSW Health Guidelines.
On some occasions the placenta may be sent to the Pathology Department, for extra information. If you would like to take your placenta home please talk to your midwife.
Stem cell collection and storage
If you are interested in the collection of stem cells from your baby’s cord blood for possible future use, you need to organise this with one of the private companies several weeks before coming to hospital to birth your baby. You will need to organise the collection, equipment, courier service and storage with the private company.
Options of care during pregnancy
Options of care during pregnancy
GP Obstetrician
Gunnedah has a GP obstetrician led model of care. All antenatal visits are conducted by your GP.
Specialist Obstetric Care at Gunnedah Hospital Antenatal Clinic
Specialist Obstetricians are best able to care for women who have pregnancies complicated by:
- Had a previous pregnancy requiring specialist care and/or hospitalisation
- A pregnancy that is not progressing normally
- A multiple pregnancy, e.g. twins
- Diabetes and/or other conditions
In this instance, your GP would refer you to either Tamworth or John Hunter Hospital for specialist care.
AMHIS (Aboriginal Maternal Infant Health Service)
Gunnedah provides care for Aboriginal and Torres Strait Islander women, and/or women whose baby will be Aboriginal and Torres Strait Islander. The Kadeekamballa clinic aims to provide culturally appropriate support and education during pregnancy and after birth. This service includes antenatal care, child and family health care, child health checks, support service referrals and health education and operates on a Thursday afternoon (no appointment required). You may contact the staff at Kadeekamballa directly, or talk to your GP to make a referral to our service.
Please contact : phone no (02) 67418090 or 67418000
Pregnancy support service
Pregnancy support services
Multicultural Health Services
The Multicultural Health Unit provides the following services to women from culturally and linguistically diverse (CALD) backgrounds:
- Health Care Interpreter Services
The Multicultural Health Unit provides professional health care interpreters for all women from CALD backgrounds. Health Care Interpreters assist women to communicate with their health professional during antenatal visits, classes, labour, postnatal period and other health-related occasions. If you need the assistance of a health care interpreter please let staff know and they will book one for your appointment.
Aboriginal Liaison Officers
The Gunnedah Hospital Aboriginal Liaison Officer is available to assist Aboriginal and Torres Strait Islander patients.
If you or your family require assistance in accessing hospital services, please ask one of our staff members to contact the Aboriginal Liaison Officer for you.
Care and Support for women with drug and alcohol problems
Some women may still be using alcohol or taking drugs during pregnancy. It is known that this can be very harmful to the unborn child. A number of skilled, non-judgmental and empathetic staff can provide a range of support. This will greatly improve the chances of having a healthy baby. Other services include the Drug and Alcohol Team and Social Work team.
Providing practical assistance and counselling: Social Work
Social workers are part of the health care team looking after you and your family while you are in hospital.
Social Workers can offer counselling to individuals and families in all areas, including:
- Women or families experiencing difficulties during the pregnancy, such as family breakdown or financial difficulties
- Women or families considering adoption
- Information about community support services
If you wish to contact a social worker, you can contact the Social Work Department directly on (02) 67418105 or ask your midwife, doctor or other hospital staff involved in your care to contact a social worker for you.
Promoting Healthy Eating: Dietitians
Both you and your baby need extra nutrients during all stages of pregnancy and breastfeeding. Eating a nutritious diet during pregnancy promotes healthy growth and development for your baby, prepares you for breastfeeding and is important for your own wellbeing. It is important to remember that even though you are eating for two, there is no need to eat twice as much.
A dietitian can assess your diet and suggest any changes that you may need to make. This is particularly important for women who are under- or over-weight, suffer from anaemia or a malabsorption illness such as Crohn’s or Coeliac disease, follow a vegetarian diet, or are diabetic.
You can arrange to see the dietitian by asking a midwife during your Booking – in visit or hospital stay.
Get Healthy in Pregnancy
The Get Healthy in Pregnancy Service is a FREE telephone health coaching service available to anyone aged 16 years and over. You will be able to talk with a qualified dietitian or exercise physiologist over the phone in the privacy of your own home.
Your health coach could help you to:
- Eat healthily
- Get active
- Gain or maintain a healthy amount of weight during your pregnancy
- Not drink alcohol during your pregnancy
- Return to your pre-pregnancy weight.
For Aboriginal women or women carrying an Aboriginal baby you may be able to speak with the Get Healthy Aboriginal Liaison Officer, for your first phone call or one of your coaching calls. The ALO will talk to you about your needs and your access to services in the community before referring you to either a dietitian or an exercise physiologist for the remainder of your phone calls.
Discuss referral to the service with your midwife at your booking-in visit or you can click the image below for more information and to refer yourself to the service.
This service can be accessed online or discuss referral with the midwife at your booking in visit.
Helping women to move well: Physiotherapy
A physiotherapist is available to give you advice or treatment on the discomforts that may arise during your pregnancy or after your baby is born. These may include back pain, pelvic pain, pelvic floor weakness, incontinence or abdominal muscle weakness.
If you wish to see a physiotherapist, contact them directly by phoning 0267418093 or ask your caregiver to contact them for you.
Pregnancy Information
When should you contact the hospital
When you should contact Gunnedah Hospital
Please phone Gunnedah Maternity Unit 6741 8037 immediately for advice if any of these occur:
- Your baby stops moving or there is an obvious reduction in your baby’s movements at any time during your pregnancy
- Trauma to the abdomen, assault, serious fall or car accident
- Vaginal bleeding at any time
- Sharp pains in the abdomen with or without vaginal bleeding
- Your waters break or if you have a constant clear watery vaginal discharge
- Fever or chills, temperature over 37.8 degrees
- Severe nausea and persistent vomiting
- Recurring and persistent headaches
- Blurred vision or spots before your eyes
- Pain or burning on passing urine
- Contractions at any time before 37 weeks
- Sudden swelling of the face, hands or feet
- Persistently itchy skin, especially hands and feet
- Labour has started and you feel it is time to come to hospital
- Booked Caesarean birth and labour commences
Antenatal clinic general information
Antenatal clinic general information
The first Booking-in antenatal visit
All women will have their first visit with a midwife. This is a comprehensive visit where we will discuss your previous medical history, family medical history, and your general well-being. This is to determine ways we can provide you with appropriate care and support throughout your pregnancy and to ensure your pregnancy care meets your needs.
You can expect your first appointment to take about one hour. Please arrive at the clinic at least 10 minutes prior to your appointment time, this will allow time to complete your paperwork before you see the midwife. Your partner or support person is always welcome at your visits, but due to the length and personal nature of your first visit, we ask that you attend this appointment alone where possible.
Booking-in to hospital (admission procedures)
This is different to the antenatal ‘Booking-in’ visit. All hospital inpatients must complete admission procedures, including details of Medicare card, any health insurance, next of kin, etc. As pregnant women know they will be inpatients at some time in the near future, it is suggested that these are completed well ahead of the baby’s due birth date.
Ultrasound and pathology results
Routine antenatal care involves blood and urine tests, and ultrasounds examinations. These test results are made available to you at your next antenatal visit appointment. All abnormal results that require follow up will be communicated to you by your care provider. We ask that, where possible, that you do not phone for test results.
Students at Gunnedah
The Gunnedah hospital provides important training opportunities for student Midwives. Students are always under the direct supervision of an experienced Midwife. You will be asked permission before a student observes or participates in your care and you have the right to say no. Your wishes will be respected at all times and this will not affect your care.
Our future midwives, the midwifery students, are available to share your pregnancy journey with you, and can provide a familiar face throughout your pregnancy, birth and postnatal experience. Speak to your midwife if you would like to be part of this special program.
Overseas Visitors or those who don’t have a Medicare card
The Gunnedah Hospital is a public health care facility. All patients must have a Medicare card. Women not eligible for Medicare benefits will be asked to pay a fee at each visit; this may be reimbursed later by their own Health Insurance Fund.
General information for Maternity Inpatients
What to bring to hospital when having your baby
Please bring all you need for yourself and your baby for one day in 1-2 small overnight bags, as space is limited in the hospital.
For the mother
- Antenatal Record
- You are encouraged to wear your own clothes during labour and birth. A comfortable cotton nightshirt or long T-shirt or sarongs are suitable (you may need more than one if you wish to be covered while in the shower or bath)
- Comfortable underwear
- Sanitary adhesive pads
- Maternity bras or “crop top,” breast (nursing) pads (disposable or cloth, not plastic lined)
- Comfortable clothing, suitable when breastfeeding: T-shirts, shorts/trousers or leggings for day wear, pyjamas, nightshirts,
dressing gown - Non slip footwear
- Toiletries, tissues, etc
- Massage oil
- Your favourite food and drink to keep up your energy levels, preferably these should be non perishable; special foods that require cooling or heating must be carried and stored following Safe Food Handling Guidelines
- MP3 or iPod, with selection of music, relaxation and/or affirmations for different stages of labour; some speakers available, but you may bring your own, labelled (all optional but may be helpful)
- Mobile phone
- Camera or smart phone (still photos only)
- Note pad/ book and pen
- Please leave all valuables at home – there is nowhere to secure them safely in the hospital
For the Support person
- Wear ‘closed’ shoes for WH&S safety in the Birthing Service
- Change of clothes/board shorts if assisting mother in shower or bath
- Jacket or warm clothing for cool air conditioning
- Snacks and drinks (following Safe Food Handling Guidelines)
- Toothbrush & paste
For baby
- An outfit to go home
- Gunnedah Maternity provides baby singlets, gowns, and cloth nappies, bunny rugs, bonnets and bootees during the stay.
- Optional: bath solution or baby soap, baby lotion or wipes (just water for baby is fine)
- Disposable nappies if desired, although staff may suggest cloth to assess fluid status.
- If you are formula feeding your baby, bring a tin of your choice of infant formula, bottles and teats. The hospital uses Milton solution to sterilise bottles and teats but does have a microwave if steam steriliser is used.
- An approved baby restraint as required by law should be fitted to your car; it is strongly suggested that you do this when you are about 34-36 weeks pregnant. If you need help with this, check the Transport NSW website for fitting stations located near you.
Mother and Baby Care Boards
 Near each bed you will notice a Mother and Baby Care Board. We use
Near each bed you will notice a Mother and Baby Care Board. We use these boards in all ward areas across the hospital to communicate the daily and anticipated plan for care between the woman, the family and carer and healthcare team.
these boards in all ward areas across the hospital to communicate the daily and anticipated plan for care between the woman, the family and carer and healthcare team.
Ward staff will update the board each shift, and you or your family or carer can write comments and questions on it at any time. If you have any questions regarding your care board, please ask one of our staff members. For your safety, we want to work together to plan your care and know what is important to you.
PLEASE INFORM US WHEN YOU LEAVE THE WARD
We need to check if there is anything we should do for you before you go, and confirm what time you plan to return.
REACH: Recognise, Engage, Act, Call, Help
If you or a family member becomes concerned about your condition while in hospital:
- Have you spoken to your midwife or doctor?
- Have your concerns been answered?
- Are you still concerned?
If so, ask your midwife for a ‘Clinical Review’, or you can dial 0428628354 in business hours and 67678195 to call an emergency response.
A REACH poster will be displayed beside your bed with this information.
Clinical handover
At Gunnedah Maternity we aim to provide excellent healthcare for every woman, every time. An important part of this commitment is staff performing a clinical handover at the bedside morning and afternoon shift.
At the handover, the midwife who has been caring for you provides information regarding your care and reason for your admission to the midwife who will be looking after you during the next shift.
The staff will involve you in this process, which will allow you to participate in the planning of your care and ensure that the information that is exchanged is accurate. You will also have an opportunity at this time to ask any questions regarding your care.
Hand Hygiene
To help prevent infection the following rules are for all visitors for the Gunnedah Hospital:
- Gel hands on entering unit
- Gel hands on entering patient’s rooms
- Gel hands on exit from patient’s room
- Inform staff if you are unwell
- Wear a mask at all times
Providing a safe environment for clients and staff
Creating a safe environment for patients, visitors to our hospital and our staff is our priority. Any behaviour which compromises the safety of mothers and babies will not be tolerated. Any behaviour which disrupts the ability of our staff to fulfil their duty of care will also not be tolerated.
Should any person display such behaviour they may be asked to leave.
Security
The hospital has a lock down period between 8pm and 7am. During these hours, entrance and exit to Gunnedah Hospital is via the Emergency Department entrance only.
Security cameras are located in most areas throughout the hospital.
Belongings and Valuables
To minimise the chance of misplacing your belongings it is helpful if your items are marked with an identifying label, especially valuables such as glasses and phone chargers.
We do our best to ensure all private items are returned to you if misplaced but we cannot take responsibility for lost items. Valuable items are best left at home for safekeeping. There is no secure environment on the wards to store valuable items.
Car Parking
Car parking is available at Gunnedah Hospital.
Visiting Hours
Gunnedah Maternity’s visiting hours are from 11am to 8pm. We acknowledge that new mothers need rest and so we encourage a rest period on the wards between 1pm and 3pm each day.
The majority of our beds are in two-bed rooms, so when visiting we ask that you are mindful of respecting the other women and babies on the ward.
We also request that visitors are up-to-date with the whooping cough vaccination when visiting new babies, and if feeling unwell with colds and flu-like illness, please avoid visiting new mothers and babies.
Smoke Free Health Service
Gunnedah Hospital is a smoke-free health service. Smoking is not permitted in the hospital or on hospital grounds. The midwife caring for you will assist you with smoking cessation support if required.
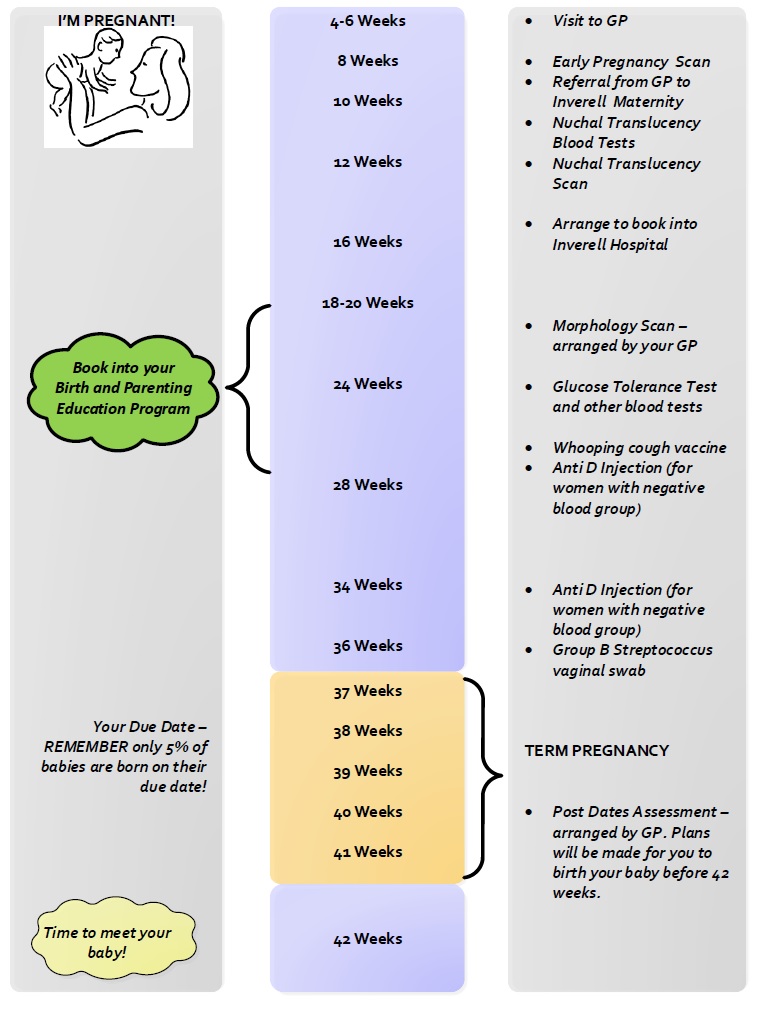
Normal pregnancy timeline
Preparing for Parenting
The Parenting Education Service
Gunnedah Parenting Education Service
“Knowledge reduces fear and promotes confidence”
Learning about your pregnancy and growing baby, preparing for labour and the birth of your baby, preparing for the joys and challenges of becoming a parent are all very important parts of your antenatal care and planning.
The Gunnedah Hospital Parenting Education Service offers antenatal education programs to support you and your partner with your physical, mental and emotional preparation for your pregnancy, birth, early parenting and feeding your baby.
The sessions are relaxed and informative, giving you and your support person the opportunity to meet other families and discuss ideas, thoughts and choices for birthing and parenting.
It is important to book your sessions early to ensure you don’t miss out on a time that best suits you.
Why come to our programs?
Attending face to face education programs will help you to learn more about your birth and parenting journey as we are able to tailor our programs to meet your specific learning needs. You will share the experience with other pregnant women and families which is an excellent parent-education to meet others about to become new parents.
Our qualified, welcoming team will provide an environment which is informal and relaxed. Our programs are interactive and based on the most up to date information.
General information about educational programs
Courses are held at Gunnedah Hospital in accordance with demand (usually a one day session on a Saturday).
Booking Information
Your Booking- in Midwife can assist with booking arrangements or alternatively contact the Hospital Administration now to book your place
Phone: 0267418037
Schedule of Programs
Birth and Parenting Program
- Self-help strategies for labour and birth, including ways that the support person can offer support to the laboring woman.
- Understanding labour and birth, including when to come to hospital.
- Making informed decisions about your care, unexpected events of labour and after the birth.
- Breastfeeding, infant sleep, settling techniques, infant communication & other baby care topics.
- Changes in the family relationships during the period of the transition to parenthood.
| Date | Class Times | Duration | Status |
|---|---|---|---|
| Saturday 22nd June and Sunday 23rd June 2024 | 8.30am - 2.30pm | whole weekend | AVAILABLE |
| Saturday 3rd August and Sunday 4th August 2024 | 8.30am - 2.30pm | whole weekend | AVAILABLE |
Our past clients say
“I felt prepared for anything !”
“Good time out from our busy lives to focus on the pregnancy as a couple; it reinforced what we read on internet; partner found it very helpful.”
“Fantastic to meet & share with others at the same stage of pregnancy & share questions about birth, reduced the fear about what we were facing; we are still in touch with our group on facebook.”
Online Live Streamed programs
HNE Health are offering interactive online live streamed programs by an experienced Healthcare Professional who will help engage with your online group through all aspects of pregnancy, birth and early parenting.
Our previous clients say.....
"We learn't alot about labour and options during the process. An incredibly informative course and very interactive so we could retain the information! We loved it."
"We had very little knowledge prior to this course. This course has covered a wide range of topics and provided additional sources for us to get further information."
To see available online classes, click here
After baby arrives
Postnatal unit
Gunnedah Postnatal Unit
During your stay on the postnatal ward, you will be supported by midwives who will assist you to develop the skills to care for your baby. There are opportunities for inpatient education sessions on the ward such a baby bathing demonstration. These are all great opportunities to gain confidence as new parents.
When you first arrive to the postnatal ward, the midwife caring for you will discuss a plan of care for your stay including discharge planning.
Accommodation options
For most women, pregnancy and birth is a healthy experience, which does not necessitate a long stay in hospital.
The Maternity ward at Gunnedah Hospital is a 9 bed combined antenatal and postnatal ward and has mostly shared two bed rooms. This means that family members are unable to stay overnight with the mother and baby. There is 1 single room available. Women with more complicated antenatal or postnatal stays are allocated to the single room as first priority. We also attempt to meet the needs of women who have private health insurance by offering a single room whenever possible.
Rooming-in
It is important not to separate mothers from their babies, so mothers keep their baby at the bedside with them, 24 hours a day. The midwives will assist and provide support with all aspects of baby’s care. Please ask for assistance if required. There is also a Mother and Baby Care Board near each bed which is a very useful way to request support.
Feeding your baby
The midwives caring for you are able to give assistance, support and advice with breastfeeding.
If you are artificially feeding your baby, you will need to bring a tin of your choice of infant formula with you, sterile bottles and teats, to use in hospital. We provide sterilisation of equipment with Milton solution or microwave steam steriliser.
Support for breastfeeding your baby when you go home
Kaleidoscope (Child and Family Health Nursing Service) provide Breastfeeding Clinics in larger communities.
- The Australian Breastfeeding Association (ABA) provides breastfeeding support in the community. 24-hour phone number: 1800 6862686 (1800 MUM 2 MUM); while membership supports this valuable organisation, non-members can still receive support.
- Child and Family Health Nurse provides long-term ongoing feeding and parenting support. You will be linked to this free service before discharge from our maternity service.
- Look for Who Can I Call? Refer to your baby’s blue book for useful phone numbers.
Physiotherapy after your birth
If required, your midwife may refer you to our physiotherapist who will see you while in hospital or as an outpatient. For further information, phone physiotherapy on (02) 67418093 or ask your midwife.
Routine screening for your baby
Routine screening as outlined in the NSW Health Having a Baby book will be done in the early postnatal days.
You will be offered a screening test for hearing for your baby soon after birth. About one to two babies out of every 1000 will have a significant hearing loss. This screening program is called the NSW State-wide Infant Screening Hearing program (SWISH), and is available in the postnatal ward at your local Early Childhood and Family Centre if you go home early.
Newborn Bloodspot Screening will be done around day 3-4 by your midwife or a pathology technician.
Transport for going home
Please plan for your transport home. You will need an approved baby restraint fitted to your car. Ideally this should be in place around 34-36 weeks pregnant. The Transport NSW website can help you locate a fitting station near you.
Discharging Home
Discuss with your midwife your needs for discharge. Ensure that you arrange on the previous evening for someone to collect you.
Postnatal timeline
| Time after birth of baby | Care for baby | Care for mother |
|---|---|---|
| Birth day | Vitamin K (Konakion) Immunisation - Hepatitis B Newborn baby check
| Consent required |
| 1-5 days | Hearing check
| Consent required |
| 1-5 days | Hip check
| Consent required |
| 3-4 days | Newborn bloodspot screen
| Signed consent required |
| Approx 2 weeks | Home visit by Child and Family Health Nurse (C&FHN)
| |
| 2 weeks | Visit your GP
| Mother might discuss contraception or other issues |
| 6 weeks | Visit your GP
|
|
Keeping you and your baby safe while in hospital
Keeping you and your baby safe while in hospital
Sometimes mothers to be and new mothers can fall while in hospital and cause injury particularly if they are tired, or if they have recently had an anaesthetic (including an epidural), pain medication or heavy bleeding or if the mum to be or new mum has other medical conditions such as low blood pressure, epilepsy or diabetes.
We request that you:
- Use your call bell if you require assistance
- Wear safe footwear at all times
- Take your time when moving about
- Use a shower chair when showering
- Use a light as required during the night time.
It’s important also to keep your baby safe from falling. We ask you to ensure that your baby:
- Is placed on their back to sleep and placed in their own cot placed next to your bed
- Is never left unattended on an adult bed or other surface from which they can fall
- Is always in their own cot while being transported. Walking around with your baby in your arms is not encouraged.
We Do Not Encourage Sleeping With Your Baby As Babies Can Fall Or Have Sleep Accidents
Please ensure that visitors are aware of these important factors to keep your baby safe.
We recognise that babies like to feel safe in their mum’s arms, but sometimes tired mums can fall asleep with their babies and babies can then easily fall from their mums’ hold. We ask that you avoid all of these situations that place your baby at risk of falls.
REMEMBER the safe sleeping SIDS prevention = Baby on back, in own bed, feet at end of cot, smoke free environment, no hats or bonnets, and breastfeed your baby.
See more at https://rednose.com.au/section/safe-sleeping
After birth care
After birth care
Contraception
It is possible to fall pregnant immediately after giving birth even if you are breastfeeding.
If you do not desire to fall pregnant then consider using barrier contraception (condoms). You may resume sexual activity as soon as you feel comfortable. You may need to wait longer if you had a vaginal birth requiring stitches, or a caesarean birth.
If you are breastfeeding then it is important not to start the combined oral contraceptive pill as it may affect your milk supply. Your options will include progesterone-only pills (the mini pill), a progesterone implant or progesterone injection given every third month.
Ask your GP for more information at your six-week appointment.
Feeling unwell
If you are feeling unwell please contact your GP or local Maternity Service.
General signs of infection include:
- Pain
- Redness
- Swelling
- Discharge that may have an unpleasant odour
- Temperature
- Area may be hot to touch
If you are breastfeeding and find painful areas that are red and lumpy you may have blocked milk ducts or be developing mastitis (infection of the milk ducts).
In this case you should to see your GP as soon as possible, however keep breastfeeding/expressing for until your appointment time as it may help to relieve the blockage.
Postnatal follow up with your GP
We recommend that you and your baby visit your local GP within six weeks after birth.
A full complete postnatal review should be attended at this appointment which may include:
- Your baby should have a complete routine head-to-toe check up
- Discuss contraception with you GP
- Have a plan when your next pap smear is due
- Discuss current medications and follow-up scripts required
- Have perineal suturing reviewed or Caesarean wound check
- Discuss any discomforts that you may be experiencing including incontinence
- Discuss your emotional well being
- Blood tests (as required)
- Breast check
- Blood pressure
- Pap smear
- Perineal stitches or caesarean section wound
- Discuss any incontinence you may be experiencing
- Emotional well being