Maternity Services at Glen Innes Hospital
Congratulations on your pregnancy and welcome to the Glen Innes Hospital Birthing Service.
Welcome to the Glen Innes Hospital Maternity Unit Information for women and their families.
"We would like to acknowledge the Traditional Custodians and community members of the land Glen Innes Hospital is situated on, The Ngarabal People, and pay our respects to Elders, past, present and those emerging"
Our Maternity group practice program in Glen Innes offers all risk antenatal care with one midwife (who works in a team). Your midwife will care for you in your pregnancy and at home for up to 6 weeks after your baby is born.
Our focus for maternity care is to ensure that it is collaborative, where the woman and her family remain at the centre of the care experience and are actively involved in all decisions about the pregnancy, birth and after your baby is born. All decision making is based on relationships of mutual respect and trust.
Please click here to learn more about your Rights and Responsibilities as a patient, carer or community member of the Hunter New England Local Health District
Download the NSW Health Having a Baby Book here
| Glen Innes Telephone Numbers: | |
| Maternity Unit | 0267390226 |
| Birth & Parenting programs (Parenting Education Service) | 0267390226 |
| Aboriginal Maternal Infant Health Service | 0439493039 or 0267219594 |
Pregnancy Care at Glen Innes
Now that you are pregnant
Now that you are pregnant
Your care begins with your General Practitioner (GP), by confirming your pregnancy, taking a comprehensive health and medical history, ordering your blood tests and an obstetric ultrasound.
comprehensive health and medical history, ordering your blood tests and an obstetric ultrasound.
Your GP will write and send a referral to the Glen Innes Hospital maternity unit to initiate your care and is usually done at around 11 -14 weeks or you can contact Glen Innes maternity around 11-14 weeks.
Once we have received your completed referral, including all blood test results and scan reports, our maternity unit will then process your details and notify you by phone to make an appointment time to have a booking in visit. This visit will be attended by a midwife at either Glen Innes maternity unit and usually occurs between 11-14 weeks. During this visit, the midwife will discuss with you the options of care available for your pregnancy.
Where you have your pregnancy care will depend on your general health, your preferences, where you live and your previous birth experience.
The midwife will also discuss the importance of healthy eating and physical activity during this visit. You will be offered a referral to the Get Healthy in Pregnancy service. The Service is open to anyone aged 16 years and over. You will be able to talk with a qualified dietitian or exercise physiologist over the phone in the privacy of your own home. For Aboriginal women or women carrying an Aboriginal baby you may be able to speak with the Get Healthy Aboriginal Liaison Officer (ALO), for your first phone call or one of your coaching calls. The ALO will talk to you about your needs and your access to services in the community before referring you to either a dietitian or an exercise physiologist for the remainder of your phone calls.
Click on the image below for more information or to refer yourself to the service.
Options of care during pregnancy
Options of care during pregnancy
Midwifery Group Practice (MGP)
This model of care is provided by a team of midwives at Glen Innes Hospital. The MGP program offers you one midwife (who works in a team) who will care for you in your pregnancy and at home for up to 6 weeks after your baby is born. Your midwife will support you with active labour, normal birth, breastfeeding and early discharge from the birthing unit.
The Midwives consult with a local GP obstetrician, Obstetricians in Armidale, Tamworth or JHH according to your individual health and pregnancy needs.
You will need to come to the maternity unit for a Booking-in visit between 11-14 weeks with a midwife. Your baby will be born at Glen Innes Hospital unless certain pregnancy complications arise.
Specialist Obstetric Care at Armidale Hospital Antenatal Clinic
Specialist Obstetricians are best able to care for women who have pregnancies complicated by:
- A previous pregnancy requiring specialist care and/or hospitalisation
- A pregnancy that is not progressing normally
- A multiple pregnancy, e.g. twins
- Diabetes and/or other conditions
This care is accessible at Armidale Hospital and may involve shared care with your local GP.
AMHIS (Aboriginal Maternal Infant Health Service)
The AMIHS provides care for Aboriginal and Torres Strait Islander women, and/or women whose baby will be Aboriginal and Torres Strait Islander. The service aims to provide culturally appropriate support and education during pregnancy, after birth and for children up to early school years. This service includes antenatal care, child and family health care, immunisation, child health checks, support service referrals and health education. It is a shared service with Inverell hospital. You may contact the staff directly, or talk to your GP to make a referral to the AMHIS service.
Please phone AMIHS on 0439493039 OR 0267219594
- You think you are pregnant or have a positive pregnancy test
- You have children between 0-5 years
Summary of options of care
| Options of care | Suitability | Who will provide your antenatal car | Where you will have your antenatal care | Who will provide care during labour and birth |
|---|---|---|---|---|
| Midwifery Group Practice (MGP) | All risk antenatal care and for women with uncomplicated pregnancy, labour and birth care | A midwife | Glen Innes Maternity Unit | MGP midwife |
| Shared Care AMIHS Service | Aboriginal and Torres Strait Island women or women having an Aboriginal and Torres Strait Island baby | AMIHS midwives | Home | Glen Innes Hospital Midwife |
| Shared Care with GP and Consultant Obstetrician | Women with complicated pregnancy | GP of your choice; midwife at Booking-in and Consultant at Referral Hospital (Armidale, Tamworth or JHH) | Decided on individual care needs | If birthing at a referral hospital the birth suite midwife |
Pregnancy support service
Pregnancy support services
Early Pregnancy Assessment Service
This service is available for women with early pregnancy abdominal pain, bleeding or severe vomiting (up to 18 weeks) through the midwifery group practice team.
Multicultural Health Services
The Multicultural Health Unit provides the following services to women from culturally and linguistically diverse (CALD) backgrounds:
- Health Care Interpreter Services
The Multicultural Health Unit provides professional health care interpreters for all women from CALD backgrounds. Health Care Interpreters assist women to communicate with their health professional during antenatal visits, classes, labour, postnatal period and other health-related occasions. If you need the assistance of a health care interpreter please let staff know and they will book one for your appointment.
- Aboriginal Liaison Officers
The Glen Innes Hospital Aboriginal Liaison Officer is available to assist Aboriginal and Torres Strait Islander patients.
If you or your family require assistance in accessing hospital services, please ask one of our staff members to contact the Aboriginal Liaison Officer for you.
Care and Support for women with drug and alcohol problems
Some women may still be using alcohol or taking drugs during pregnancy. It is known that this can be very harmful to the unborn child. A number of skilled, non-judgmental and empathetic staff can provide a range of support. This will greatly improve the chances of having a healthy baby. Other services include the Drug and Alcohol Team and Social Work team.
Providing practical assistance and counselling: Social Work
Social workers are part of the health care team looking after you and your family while you are in hospital.
Social Workers can offer counselling to individuals and families in all areas, including:
- Women or families experiencing difficulties during the pregnancy, such as family breakdown or financial difficulties
- Women or families considering adoption
- Information about community support services
If you wish to contact a social worker, ask your midwife, doctor or other hospital staff involved in your care to contact a social worker for you.
Promoting Healthy Eating: Dietitians
Both you and your baby need extra nutrients during all stages of pregnancy and breastfeeding. Eating a nutritious diet during pregnancy promotes healthy growth and development for your baby, prepares you for breastfeeding and is important for your own wellbeing. It is important to remember that even though you are eating for two, there is no need to eat twice as much.
A dietitian can assess your diet and suggest any changes that you may need to make. This is particularly important for women who are under- or over-weight, suffer from anaemia or a malabsorption illness such as Crohn’s or Coeliac disease, follow a vegetarian diet, or are diabetic.
Our staff can refer to this service as required or requested.
Get Healthy in Pregnancy
The Get Healthy in Pregnancy Service is a FREE telephone health coaching service available to anyone aged 16 years and over. You will be able to talk with a qualified dietitian or exercise physiologist over the phone in the privacy of your own home.
Your health coach could help you to:
- Eat healthily
- Get active
- Gain or maintain a healthy amount of weight during your pregnancy
- Not drink alcohol during your pregnancy
- Return to your pre-pregnancy weight.
For Aboriginal women or women carrying an Aboriginal baby you may be able to speak with the Get Healthy Aboriginal Liaison Officer, for your first phone call or one of your coaching calls. The ALO will talk to you about your needs and your access to services in the community before referring you to either a dietitian or an exercise physiologist for the remainder of your phone calls.
Discuss referral to the service with your midwife at your booking-in visit or you can click the image below for more information and to refer yourself to the service.
This service can be accessed online or discuss referral with the midwife at your booking in visit.
Helping women to move well: Physiotherapy
A physiotherapist is available to give you advice or treatment on the discomforts that may arise during your pregnancy or after your baby is born. These may include back pain, pelvic pain, pelvic floor weakness, incontinence or abdominal muscle weakness.
If you wish to see a physiotherapist, ask your caregiver to contact them for you.
Glen Innes Birth suite
Glen Innes Birth Suite
The Glen Innes maternity unit is located on first floor, eastern side of the building. When you arrive at the hospital go to the first floor and follow the signs to the maternity unit or call your known midwife. You will be met by a midwife who will take you to an available room.
A plan for going home after birth
For most women, pregnancy and birth is a healthy experience. Women may choose to go home from the hospital soon after the baby is born. This is dependent on both mother and baby being well, baby has had the first feed, and mother is confident going home with adequate family support. You can go home straight from Birth Suite. A physical examination of mother and baby will be done before you leave. All the necessary documents and supportive information will also be provided.
Travelling to have your baby in hospital
- Contact the midwife in the Birthing Service for advice.
- Wear a sanitary pad
- Have your support person drive safely, and use your seat belt with lap belt positioned below your baby. Have old towels available to catch leaks if they occur, and an old ice-cream bucket in case of nausea or vomiting.
- In NSW, an ambulance ride can be very expensive; it is strongly suggested that you join an ambulance fund for your family emergency situations, if you are not already covered by private health insurance (this may be done through any major private health fund office or online).
- Bring your antenatal record. Your antenatal record provides us with your history and plan of management for labour and birth. Please carry it at all times, and present it to the midwife on your arrival.
Husband/ partner/ support persons in labour and birth
We welcome people who will support and encourage you throughout labour and birth. There is room for a maximum of two support people at any one time in the Birth Suite.
Doulas
It is the woman’s choice who supports her during pregnancy, labour, birth and the postnatal period. A doula is a layperson, identified by the woman, who provides continuous support during the antenatal period, childbirth and the postnatal period. The doula attends as an employee of the woman.
Hunter New England Local Health District (HNELHD) is open to the use of doulas at birth, and maternity services will facilitate a productive, receptive environment for doulas to support women. However, HNELHD clearly states that it does not accept responsibility and is not accountable for any actions or advice given to labouring women by doulas.
Visitors
You may wish to have some visitors visit you soon after the birth of your baby in the Birth Suite, they may present to the maternity unit and notify staff that they have arrives. This is to protect your privacy and the privacy of other women in the unit. Please be aware that there is no waiting room for visitors in the Birth Suite.
Enquiries while in Birth Suite
To protect your privacy and confidentiality, information is not given to people enquiring about you without your consent. We will take messages for you to contact the enquirers at a convenient time.
Video recording and photography
We respect your wish to film labour and birth. However, all staff have the right to refuse to be identified on film or refuse filming during specific procedures. Please inform your midwife of your intention to film.
Children
There are no childcare facilities available in the maternity unit. If you wish to have your children present for labour and birth, we request you have one adult, other than your main support person to care and supervise. However, the limit of two additional people at a time will also need to be considered.
Mobile phones
We ask that all mobile phones are turned to silent mode in the Birth Suite, and ward environments.
Keeping baby with you following birth
Your baby will remain with you following birth. Skin-to-skin is encouraged for a minimum of 1 hour after the birth or until the first breastfeed. Skin to skin contact stimulates the mothers’ production of the oxytocin hormone, which decreases bleeding, promotes bonding and breastfeeding. It allows the baby to smell, touch and know mum as well as stay warm. When the baby shows signs of readiness, he/she will be able to breastfeed.
It is strongly suggested that during this important time the baby stays with mum, rather than being handed around to other family members. The father of the baby has an important role in protecting the new mother and baby.
After your baby has fed, he / she will be weighed and measured. With your consent, Vitamin K (Konakion) and Hepatitis B vaccine injections will be given at this time.
Two arm-bands with the baby’s correct identification details will be placed on the baby’s arm and leg – the midwife will ask you to check these details to ensure they are accurate. The identifying number on the mother’s armbands are the same as the baby’s, so it is important that you make sure the identifying numbers correspond.
The armbands are routinely checked by the midwives. Should the armbands fall off, please tell the midwife as soon as you can so that new armbands can be provided.
What happens to the placenta (afterbirth)?
After the birth of your baby, the placenta will be disposed of in accordance with NSW Health Guidelines. You may choose to take your placenta home with you, please let the midwife know prior to birth.
On some occasions the placenta may be sent to the Pathology Department, for extra information.
Stem cell collection and storage
If you are interested in the collection of stem cells from your baby’s cord blood for possible future use, you need to organise this with one of the private companies several weeks before coming to hospital to birth your baby. You will need to organise the collection, equipment, courier service and storage with the private company.
Pregnancy Information
When should you contact the hospital
When you should contact Glen Innes hospital
Please call your known midwife or phone Glen Innes Hospital Birth Suite on 0267390226 immediately for advice if any of these occur:
- Your baby stops moving or there is an obvious reduction in your baby’s movements at any time during your pregnancy
- Trauma to the abdomen, assault, serious fall or car accident
- Vaginal bleeding at any time
- Sharp pains in the abdomen with or without vaginal bleeding
- Your waters break or if you have a constant clear watery vaginal discharge

- Fever or chills, temperature over 37.8 degrees
- Severe nausea and persistent vomiting
- Recurring and persistent headaches
- Blurred vision or spots before your eyes
- Pain or burning on passing urine
- Contractions at any time before 37 weeks
- Sudden swelling of the face, hands or feet
- Persistently itchy skin, especially hands and feet
- Labour has started and you feel it is time to come to hospital
- Booked Caesarean birth and labour commences
Antenatal clinic general information
Antenatal clinic general information
The first Booking-in antenatal visit
All women will have their booking in visit with a midwife at Glen Innes maternity unit. This is a comprehensive visit where we will discuss your previous medical history, family medical history, and your general well-being. This is to determine ways we can provide you with appropriate care and support throughout your pregnancy and to ensure your pregnancy care meets your needs.
You can expect your booking in appointment to take about one and a half hours. Please arrive at the clinic at least 10 minutes prior to your appointment time, this will allow time to complete your paperwork before you see the midwife. Your partner or support person is always welcome at your visits, but due to the length and personal nature of your first visit, we ask that you attend this appointment alone where possible.
Once you have been allocated to a model of pregnancy care (see pages 10-12), we ask that wherever possible, you ensure your appointments remain on your allocated day with your allocated doctor or midwife. This will help you receive the best care possible.
Booking-in to hospital (admission procedures)
This is different to the antenatal ‘Booking-in’ visit. All hospital inpatients must complete admission procedures, including details of Medicare card, any health insurance, next of kin, etc. As pregnant women know they will be inpatients at some time in the near future, it is suggested that these are completed well ahead of the baby’s due birth date. Booking in to hospital is generally attended at your booking in visit.
Specialty obstetric care
We have access a range of specialist services for women with broader issues that may affect their well-being during the pregnancy, including women with physical or intellectual disability, or concerns with substance use. This is in the form of a High Risk clinic which operates in Armidale. There are also specialist clinics for women with conditions such as diabetes or other medical conditions that may impact on the pregnancy or the baby’s well-being which also take place in Armidale.
These services have staff with expertise in social support, mental wellbeing, counselling, diet, physiotherapy, peer support.
If you need support from specialist services, it will be arranged by the GP providing your pregnancy care. Referral may be required to another specialist services outside of this local area, such as at John Hunter Hospital in Newcastle and will be determined on a case by case assessment.
Ultrasound and pathology results
Routine antenatal care involves blood and urine tests, and ultrasounds examinations. These test results are made available to you at your next antenatal visit appointment with your GP. All abnormal results that require follow up will be communicated to you by your care provider. We ask that, where possible, that you do not phone for test results.
Students at Glen Innes
The Glen Innes Hospital is a teaching hospital, providing important training opportunities for a wide range of health care professionals. Students are always under the direct supervision of an experienced practitioner. You will be asked permission before a student observes or participates in your care and you have the right to say no. Your wishes will be respected at all times and this will not affect your care.
Our future midwives, at times there are midwifery students available to share your pregnancy journey with you, and can provide a familiar face throughout your pregnancy, birth and postnatal experience. Speak to your midwife if you would like to be part of this special program.
Research participation
You may be invited to participate in research projects taking place at the Hospital. These projects are designed to increase our knowledge about pregnancy, birth and the postnatal period, so that we may improve our services for your care and for women in the future. Participation in research is completely voluntary. The standard of care you receive will not be affected in any way if you choose not to take part.
General information for Maternity Inpatients
What to bring to hospital when having your baby
Please bring all you need for yourself and your baby for one day in 1-2 small overnight bags, as space is limited in the hospital.
For the mother
- Antenatal Record
- You are encouraged to wear your own clothes during labour and birth. A comfortable cotton nightshirt or long T-shirt or sarongs are suitable (you may need more than one if you wish to be covered while in the shower or bath)
- Comfortable underwear
- Sanitary adhesive pads
- Maternity bras or “crop top,” breast (nursing) pads (disposable or cloth, not plastic lined)
- Comfortable clothing, suitable when breastfeeding: T-shirts, shorts/trousers or leggings for day wear, pyjamas, nightshirts,
dressing gown - Non slip footwear
- Toiletries, tissues, etc
- Massage oil
- Your favourite food and drink to keep up your energy levels, preferably these should be nonperishable; special foods that require cooling or heating must be carried and stored following Safe Food Handling Guidelines
- Phone or iPod, with selection of music, relaxation and/or affirmations for different stages of labour; some speakers available, but you may bring your own, labelled (all optional but may be helpful)
- Mobile phone
- Camera or smart phone (still photos only)
- Note pad/ book and pen
- Please leave all valuables at home – there is nowhere to secure them safely in the hospital
For the Support person
- Wear ‘closed’ shoes for WH&S safety in the Birthing Service
- Change of clothes/board shorts if assisting mother in shower or bath
- Jacket or warm clothing for cool air conditioning
- Snacks and drinks (following Safe Food Handling Guidelines)
- Toothbrush & paste
For baby
- At least three singlets
- At least three sets of clothing (every day clothes, not good ones!)
- At least three bunny rugs/baby wraps (suggest brushed cotton if cold weather, fine cotton or muslin type if warm weather)
- One packet of cotton buds (for ‘cord’ care)
- Optional: bath solution or baby soap, baby lotion or wipes (just water for baby is fine)
- Disposable nappies will be supplied during your hospital stay
- If you are formula feeding your baby, bring a tin of your choice of infant formula. Sterile bottles and teats will be provided only while you are in hospital
- An approved baby restraint as required by law should be fitted to your car; it is strongly suggested that you do this when you are about 34-36 weeks pregnant. If you need help with this, check the Transport NSW website for fitting stations located near you.
Mother and Baby Care Boards
 Near each bed you will notice a Mother and Baby Care Board. We use
Near each bed you will notice a Mother and Baby Care Board. We use these boards in all ward areas across the hospital to communicate the daily and anticipated plan for care between the woman, the family and carer and healthcare team.
these boards in all ward areas across the hospital to communicate the daily and anticipated plan for care between the woman, the family and carer and healthcare team.
Ward staff will update the board each shift, and you or your family or carer can write comments and questions on it at any time. If you have any questions regarding your care board, please ask one of our staff members. For your safety, we want to work together to plan your care and know what is important to you.
PLEASE INFORM US WHEN YOU LEAVE THE WARD
We need to check if there is anything we should do for you before you go, and confirm what time you plan to return.
REACH: Recognise, Engage, Act, Call, Help
If you or a family member becomes concerned about your condition while in hospital:
- Have you spoken to your midwife or doctor?
- Have your concerns been answered?
- Are you still concerned?
If so, ask your midwife for a ‘Clinical Review’, or you can dial 0428352807 to call an emergency response.
A REACH poster will be displayed beside your bed with this information.
Clinical handover
At Glen Innes Hospital we aim to provide excellent healthcare for every woman, every time. An important part of this commitment is staff performing a clinical handover at the bedside every shift.
At the handover, the midwife who has been caring for you provides information regarding your care and reason for your admission to the midwife who will be looking after you during the next shift.
The staff will involve you in this process, which will allow you to participate in the planning of your care and ensure that the information that is exchanged is accurate. You will also have an opportunity at this time to ask any questions regarding your care.
Hand Hygiene
To help prevent infection the following rules are for all visitors for the Muswellbrook Hospital:
- Gel hands on entering unit
- Gel hands on entering patient’s rooms
- Gel hands on exit from patient’s room
- Inform staff if you are unwell
Providing a safe environment for clients and staff
Creating a safe environment for patients, visitors to our hospital and our staff is our priority. Any behaviour which compromises the safety of mothers and babies will not be tolerated. Any behaviour which disrupts the ability of our staff to fulfil their duty of care will also not be tolerated.
Should any person display such behaviour they may be asked to leave.
Security
The hospital has a lock down period between 8pm and 7am. During these hours, entrance and exit to Birthing and Maternity Unit is via the Emergency Department only.
Security cameras are located in most areas throughout the hospital.
Belongings and Valuables
To minimise the chance of misplacing your belongings it is helpful if your items are marked with an identifying label, especially valuables such as glasses and phone chargers.
We do our best to ensure all private items are returned to you if misplaced but we cannot take responsibility for lost items. Valuable items are best left at home for safekeeping. There is no secure environment on the wards to store valuable items.
Car Parking
Car parking is available at Glen Innes Hospital at no cost. Street parking is also available around the hospital, please be aware of time restrictions in some of these areas.
Visiting Hours
Glen Innes Hospital has an open visiting policy. We acknowledge that new mothers need rest and so we encourage a rest period on the wards between 1pm and 3pm each day.
The majority of our beds are in single rooms, and one two bed room, so when visiting we ask that you are mindful of this quiet period for your family member and for other women and babies on the ward.
We also request that visitors are up-to-date with the whooping cough vaccination when visiting new babies, and if feeling unwell with colds and flu-like illness, please avoid visiting new mothers and babies
Smoke Free Health Service
Glen Innes Hospital is a smoke-free health service. Smoking is not permitted in the hospital or on hospital grounds. The midwife caring for you will assist you with smoking cessation support if required.
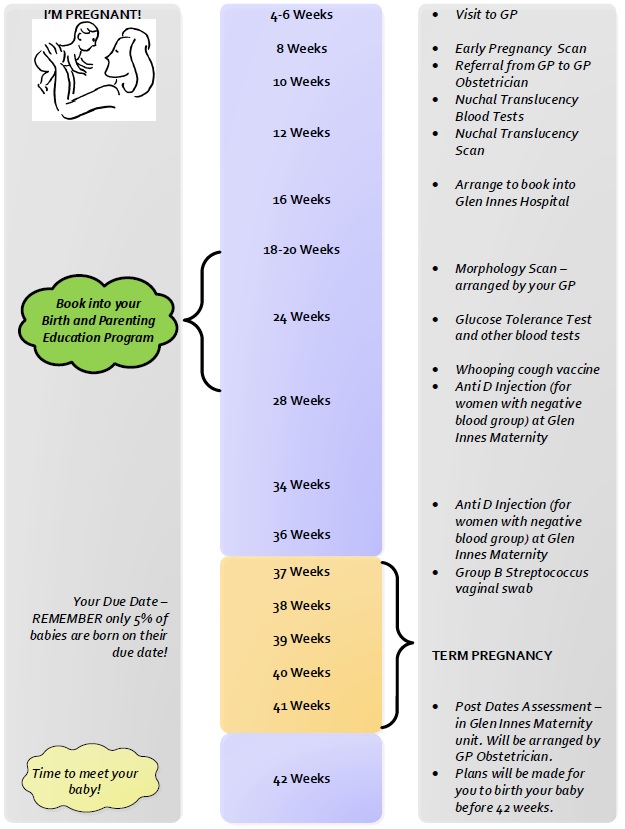
Normal pregnancy timeline
Preparing for parenting
The Parenting Education service
Glen Innes Parenting Education Service
“Knowledge reduces fear and promotes confidence”
Learning about your pregnancy and growing baby, preparing for labour and the birth of your baby, preparing for the joys and challenges of becoming a parent are all very important parts of your antenatal care and planning.
The Glen Innes Maternity Service offers the Birth and Parenting programs and Breastfeeding programs to support you and your partner with your physical, mental and emotional preparation for your pregnancy, birth, early parenting and feeding your baby.
The sessions are relaxed and informative, giving you and your support person the opportunity to meet other families and discuss ideas, thoughts and choices for birthing and parenting.
It is important to book your sessions early to ensure you don’t miss out on a time that best suits you.
Why come to our programs?
Attending face to face education programs will help you to learn more about your birth and parenting journey as we are able to tailor our programs to meet your specific learning needs. You will share the experience with other pregnant women and families which is an excellent parent-education to meet others about to become new parents.
Our qualified, welcoming team will provide an environment which is informal and relaxed. Our programs are interactive and based on the most up to date information.
Contact the maternity unit to book your place!
Office hours are: Monday to Friday 9-4pm
Phone: 0267390226
Online Live Streamed programs
Online Live Streamed programs
HNE Health are offering interactive online live streamed programs by an experienced Healthcare Professional who will help engage with your online group through all aspects of pregnancy, birth and early parenting.
Our previous clients say.....
"We learn't alot about labour and options during the process. An incredibly informative course and very interactive so we could retain the information! We loved it."
"We had very little knowledge prior to this course. This course has covered a wide range of topics and provided additional sources for us to get further information."
To see available online classes, click here
After baby arrives
Postnatal unit
Glen Innes Postnatal Unit
 During your stay on the maternity unit, you will be supported by midwives who will assist you to develop the skills to care for your baby and gain confidence as a new parent.
During your stay on the maternity unit, you will be supported by midwives who will assist you to develop the skills to care for your baby and gain confidence as a new parent.
When you first arrive to the unit, the midwife caring for you will discuss a plan of care for your stay including discharge planning.
Accommodation options
Within hours of birth, you and your baby may go home if you are both well and your baby has fed and there have been no relevant complications with pregnancy and birth. If you choose or need to stay in hospital, your care will be provided in the hospital’s maternity unit. For most women, pregnancy and birth is a healthy experience, which does not necessitate a long stay in hospital.
Rooming-in
It is important not to separate mothers from their babies, so mothers keep their baby at the bedside with them, 24 hours a day. The midwives will assist and provide support with all aspects of baby’s care. Please ask for assistance if required. There is also a Mother and Baby Care Board near each bed which is a very useful way to request support. We also ask that this board is used to communicate with the staff if you are leaving the ward for any reason. We request that you write your mobile phone number and the approximate time of your return to the ward.
Feeding your baby
The midwives caring for you are able to give assistance, support and advice with breastfeeding. Glen Innes Hospital is Baby Friendly Health Initiative (BFHI) accredited. BFHI was launched in 1991 by WHO/UNICEF, and aims to give every baby the best start in life by creating a health care environment where breastfeeding is the norm.
If you are artificially feeding your baby, you will need to bring a tin of your choice of infant formula with you, sterile bottles and teats, to use in hospital.
Support for breastfeeding your baby when you go home:
- A Breastfeeding Clinic is held weekly in the Community Health Centre. For appointments please telephone: 6542 2050
- The Australian Breastfeeding Association (ABA) provides breastfeeding support in the community. 24-hour phone number: 1800 686 268 (1800 MUM 2 MUM); while membership supports this valuable organisation, non-members can still receive support.
- Child and Family Health Nurse provides long-term ongoing feeding and parenting support. You will be linked to this free service before discharge from our maternity service.
- Look for Useful Contacts leaflet in your postnatal pack for useful phone numbers.
Routine screening for your baby
Routine screening as outlined in the NSW Health Having a Baby book will be done in the early postnatal days. You will be offered a screening test for hearing for your baby soon after birth. About one to two babies out of every 1000 will have a significant hearing loss. This screening program is called the NSW State-wide Infant Screening Hearing program (SWISH), and is available in the postnatal ward at your local Early Childhood and Family Centre if you go home early.
Newborn Bloodspot Screening will be done after 28 hours by your midwife.
Transport for going home
Please plan for your transport home. You will need an approved baby restraint fitted to your car. Ideally this should be in place around 34-36 weeks pregnant. The Transport NSW website can help you locate a fitting station near you.
Discharging Home
Please discuss with your midwife you and your babies needs for discharge home.
Postnatal timeline
| Time after birth of baby | Care for baby | Care for mother |
|---|---|---|
| Birth day | Vitamin K (Konakion) Immunisation - Hepatitis B Newborn baby check
| Consent required |
| 1-5 days | Hearing check
| Consent required |
| 3-4 days | Newborn bloodspot screen
| Signed consent required |
| Approx 2 weeks | Home visit by Child and Family Health Nurse (C&FHN)
| |
| From birth to 4-6 weeks | Midwife at home
| Mother might discuss contraception or other issues |
| 6 weeks | Visit your GP
| Postnatal check PAP smear if required Contraception discussion |
Keeping you and your baby safe while in hospital
Keeping you and your baby safe while in hospital
Sometimes mothers to be and new mothers can fall while in hospital and cause injury particularly if they are tired, or if they have recently had an anaesthetic (including an epidural), pain medication or heavy bleeding or if the mum to be or new mum has other medical conditions such as low blood pressure, epilepsy or diabetes.
We request that you:
- Use your call bell if you require assistance
- Wear safe footwear at all times
- Take your time when moving about
- Use a shower chair when showering
- Use a light as required during the night time.
It’s important also to keep your baby safe from falling. We ask you to ensure that your baby:
- Is placed on their back to sleep and placed in their own cot placed next to your bed
- Is never left unattended on an adult bed or other surface from which they can fall
- Is always in their own cot while being transported. Walking around with your baby in your arms is not encouraged.
We Do Not Encourage Sleeping With Your Baby As Babies Can Fall Or Have Sleep Accidents
Please ensure that visitors are aware of these important factors to keep your baby safe.
We recognise that babies like to feel safe in their mum’s arms, but sometimes tired mums can fall asleep with their babies and babies can then easily fall from their mums’ hold. We ask that you avoid all of these situations that place your baby at risk of falls.
REMEMBER the safe sleeping SIDS prevention = Baby on back, in own bed, feet at end of cot, smoke free environment, no hats or bonnets, and breastfeed your baby.
See more at https://rednose.com.au/section/safe-sleeping
After birth care
After birth care
Contraception
It is possible to fall pregnant immediately after giving birth even if you are breastfeeding.
If you do not desire to fall pregnant then consider using barrier contraception (condoms). You may resume sexual activity as soon as you feel comfortable. You may need to wait longer if you had a vaginal birth requiring stitches, or a caesarean birth.
If you are breastfeeding then it is important not to start the combined oral contraceptive pill as it may affect your milk supply. Your options will include progesterone-only pills (the mini pill), a progesterone implant or progesterone injection given every third month.
Ask your GP for more information at your six-week appointment.
Feeling unwell
If you are feeling unwell please contact your GP or local Maternity Service.
General signs of infection include:
- Pain
- Redness
- Swelling
- Discharge that may have an unpleasant odour
- Temperature
- Area may be hot to touch
If you are breastfeeding and find painful areas that are red and lumpy you may have blocked milk ducts or be developing mastitis (infection of the milk ducts).
In this case you should to see your GP as soon as possible, however keep breastfeeding/expressing for until your appointment time as it may help to relieve the blockage.
Postnatal follow up with your GP
We recommend that you and your baby visit your local GP within six weeks after birth.
A full complete postnatal review should be attended at this appointment which may include:
- Your baby should have a complete routine head-to-toe check up
- Discuss contraception with you GP
- Have a plan when your next pap smear is due
- Discuss current medications and follow-up scripts required
- Have perineal suturing reviewed or Caesarean wound check
- Discuss any discomforts that you may be experiencing including incontinence
- Discuss your emotional well being
- Blood tests (as required)
- Breast check
- Blood pressure
- Pap smear
- Perineal stitches or caesarean section wound
- Discuss any incontinence you may be experiencing
- Emotional well being