Improvements Achieved through Priority Initiatives
The initiatives described below are selection of the actions undertaken across Hunter New England Health District during the 2021-2022 financial year. The projects represent different clinical areas and functions of the health service, including health promotion, improving care in emergencies, preventing harm from medication errors and food allergies, improving maternity care, and ensuring our services are delivered in a culturally safe manner.
SWAP IT - Supporting parents to pack healthy school lunchboxes
SWAP IT - Supporting parents to  pack healthy school lunchboxes
pack healthy school lunchboxes
Children who are above a healthy weight are more likely to have poorer health and wellbeing, compared to children of a healthy weight. These children are also likely to carry excess weight into adulthood, placing them at increased risk of developing chronic disease in later life. Approximately one in four primary school-aged children in Australia are overweight or obese.
 Excess intake of food that is high in saturated fat, sugar, and/or salt (known as discretionary or “sometimes” foods) is known to contribute to unhealthy weight gain, and increase the risk of developing chronic diseases such as type 2 diabetes. Reducing the proportion of “sometimes foods” consumed by children, and replacing them with healthier options, “everyday foods” is the focus of SWAP IT.
Excess intake of food that is high in saturated fat, sugar, and/or salt (known as discretionary or “sometimes” foods) is known to contribute to unhealthy weight gain, and increase the risk of developing chronic diseases such as type 2 diabetes. Reducing the proportion of “sometimes foods” consumed by children, and replacing them with healthier options, “everyday foods” is the focus of SWAP IT.
SWAP IT is a program that supports parents and carers to SWAP what is packed in their child’s lunchbox from sometimes foods to everyday foods. SWAP IT has been developed through a collaboration between HNELHD Population Health and researchers from the University of Newcastle. Parents, principals, Aboriginal and multicultural representatives were involved in all aspects of the design and delivery of the program.
The SWAP IT program is primarily delivered via SkoolBag (or via usual school communication channels), an app that is widely used in Australian schools to support communication between school and home. Using an app that schools are already using allows SWAP IT to engage parents and carers in a familiar format. Parents receive weekly notifications presenting simple lunchbox swaps that can be used to replace “sometimes” foods with “everyday” foods that are healthier options. Links to further information and contact points for the local health organisation are also provided.

Over the past four years SWAP IT has been trialled and refined through multiple iterations. Research trials have shown that SWAP IT is effective in reducing the amount of unhealthy food in children’s lunchboxes. Surveys of parents and carers found that 82% of respondents regarded the SWAP IT messaging and information as helpful, and all principals at participating schools would recommend the program to other schools.
SWAP IT has already reached approximately 75,000 students in more than 180 schools across HNELHD. The program is very cost effective, and planning is currently underway to scale-up the program to schools across NSW and Australia.
TeleECG - Centralised acute coronary syndrome decision support service
TeleECG -  Centralised acute coronary syndrome decision support service
Centralised acute coronary syndrome decision support service
Acute coronary syndrome (ACS) is a term associated with sudden, reduced blood flow to the muscles of the heart. In most cases, the cause of ACS is a clot or a plaque blocking the flow of blood in the arteries that supply blood to heart muscles.
Common symptoms of ACS include discomfort in the chest and upper body, nausea, lethargy and shortness of breath. ACS is a medical emergency that can lead to permanent damage to the heart, and even heart attack. Approximately 2600 people present to emergency each month across HNELHD with symptoms of possible ACS.
Accurate and timely diagnosis of ACS can lead to reperfusion treatment, which can halve the risk of permanent cardiac damage and death. Diagnosis of ACS is made via blood tests and electrocardiogram (ECG), and the accuracy of diagnosis is influenced by the level of experience of emergency staff. National data shows that up to a third of patients miss appropriate treatment, and that missed diagnosis occurs more often in smaller emergency departments that do not have an emergency specialist on duty.

The TeleECG service supports clinicians in smaller rural hospitals across HNELHD in the diagnosis and management of patients who present with suspected ACS. The TeleECG service is staffed by specialist clinical nurse consultants who can assist in the interpretation of the patient’s ECG and blood test results, identifying patients who may be appropriate for transfer to a larger facility for reperfusion therapy. The service also provides diagnostic and management support, ensuring patients access the right care regardless of whether they present to a major tertiary hospital or a smaller rural facility.
Outcomes of the TeleECG project have been highly successful. A trial of the service found that 100% of patients who were appropriate for reperfusion therapy received this treatment, compared to 64% of patients where the TeleECG service was not in place. HNELHD is now working with the Agency for Clinical Innovation on scoping for potential state-wide implementation of the project.
ADHD Shared Care Project
ADHD Shared Care Project
Approximately 8% of children and young people (4-17years) have a diagnosis of Attention Deficit Hyperactivity Disorder (ADHD). ADHD is the most common neurodevelopmental disorder in Australia. Many young people with ADHD people rely on stimulant medication to manage symptoms such as lack of concentration, poor impulse control and hyperactivity.
Access to stimulant medications is strictly controlled under federal and state laws to limit the potential for misuse. Stimulant medications are usually prescribed by paediatricians or psychiatrists, and regular review appointments are required if a young person is to continue on these medications.
An extensive review of health services for young people in NSW, The Henry Review, called for new ways to care for young people with ADHD, so that young people could get timely access to paediatricians.
In HNELHD, it is estimated that 75% of all paediatricians’ appointments are used for ADHD medication reviews. Sometimes there are no appointments available, and the paediatrician is required to provide an extra “bridging” prescription so that the young person has enough medication until their booked appointment.
The high demand for ADHD medication reviews limits the ability of the service to see new patients in a timely manner, and leads to extended waiting times for any young person who needs to see a paediatrician. The ADHD Shared Care Project is trialling a new way to care for young people diagnosed with ADHD. In this pilot the young person can see their regular general practitioner (GP) for medication reviews, and the GP liaises with the paediatrician about care plans and medication dosages.
This means that the young person and their family can receive appropriate care closer to home, rather than travelling to the outpatient department every six months. The project promotes engagement with GPs, who are well placed to offer continuity of care and ongoing support for any other health concerns the young person has. For the health service, the aim is to free up more paediatrician appointments for new patients, reducing the amount of time young people need to wait to see a paediatrician in HNELHD.
The project is promoted through webinars, visits to GP practises, and Community HealthPathways, which a website used by GPs across the state to access referral information. The project has engaged with Armajun Aboriginal Health Service in Inverell and the Awabakal Aboriginal Medical Service (AMS) in Hamilton. An ADHD Shared Care clinic is being set up at the Awabakal AMS, where patients will be able to see their Aboriginal Health Practitioner on the same day, improving co-ordination of care and making sure that all patients have an up-to-date care plan.
Building appropriate cultural governance into the COVID-19 Pandemic Response
Building appropriate cultural governance into the COVID-19 Pandemic Response
During the initial waves of the COVID-19 pandemic in Australia there was a risk of a public health emergency developing for Aboriginal people, both in HNELHD and across the country. Aboriginal peoples are more at risk due to barriers of accessing quality and culturally safe healthcare, mobility, remoteness, crowded and inadequate housing, and high rates of chronic disease. Aboriginal people determining, developing and implementing strategies and partnering with Aboriginal health services in pandemic response planning and management is therefore very important.
The team is depicted in orange which is a healing colour. The team are portrayed as health warriors as they fight a daily battle to keep all the mobs safe. The team has created a barrier of protection as represented by the use of windbreak symbols. Beyond the protective barrier people live their lives normally while the team stand as sentinels taking on each new health challenge.
To provide guidance on how to successfully advance Aboriginal leadership and build partnerships into District processes, Aboriginal staff from the Public Health Unit developed a cultural governance model. The model is designed to facilitate a strong, representative, Aboriginal voice ranging from high level committees to teams directly supporting Aboriginal people who have COVID-19 and their contacts.
What does the Cultural Governance model look like?
Aboriginal representation and cultural oversight was included in the HNE Population Health Incident Command System (ICS). The ICS is the group that determine how to action the COVID-19 public health guidelines that are developed by the state and federal governments. Aboriginal public health staff formed the Public Health Aboriginal Team to lead, determine and guide the public health response as it relates to Aboriginal peoples. Aboriginal representatives were also incorporated into the Health Service Functional Area Coordination (HSFAC) committee, which is the lead group for the COVID-19 response across the health district. Aboriginal inclusion within Public Health ICS and HSFAC committee means that decisions and processes can be determined, assessed and implemented by Aboriginal people and ensuring they are culturally appropriate and responsive.
A wider advisory group, the HNE Aboriginal Governance Group on COVID-19, was formed that includes representatives from government, non-government, and community-controlled Aboriginal organisations. This group’s purpose is to provide cultural advice around appropriate and effective public health actions and services to support Aboriginal communities in Hunter New England. This advice and guidance is formally communicated directly to the Public Health Controller and HSFAC.
The model also included an Aboriginal Cultural Support Process for case and contact management, when all high risk cases were being contacted. This process was set up to ensure Aboriginal cases and contacts were provided with holistic care centred on cultural appropriateness. This is in addition to the usual follow-up care provided to COVID-19 cases by the health service, and was offered to any case or close contact who identified as Aboriginal or Torres Strait Islander. Between April 2020 and January 2022, the Public Health Aboriginal Team received more than 7,000 cultural support referrals, and provided cultural support to approximately 3,600 individuals. The Aboriginal Cultural Support Process has been widely shared, localised and implemented by other health districts across NSW.
The Cultural Governance model was awarded the HNELHD 2021 Excellence in Aboriginal Healthcare award.
Food Allergy Management System - Keeping patients with food allergies safe
Food Allergy Management System - Keeping patients with food allergies safe
 Food allergies can be life threatening for some patients. Modern hospitals are complex, and there are many different teams and systems involved in ordering, cooking, and delivering patients’ meals. Effective coordination between food service and clinical staff, patients and systems is vital to ensure all patients receive nutritious meals that are free from any ingredients that the patient is allergic or intolerant to.
Food allergies can be life threatening for some patients. Modern hospitals are complex, and there are many different teams and systems involved in ordering, cooking, and delivering patients’ meals. Effective coordination between food service and clinical staff, patients and systems is vital to ensure all patients receive nutritious meals that are free from any ingredients that the patient is allergic or intolerant to.
The Food Allergy Management project was set up to reduce the risks to patients who have food allergies whilst they are staying in hospitals across the district. The project represents a collaboration of staff from multiple teams including clinical groups, information technology, food services, and education and training teams. The main outcomes of the project are:
A new set of food allergy alerts have been created that can be added to patients’ electronic records. These alerts, specifically for more common and higher risk food allergens, are automatically displayed in multiple electronic applications that support inpatient care. The method of entering alerts has been improved, allowing clinicians to directly add food allergy alerts to the system instead of passing the information to administrative staff for entry. This removes double handling of information and reduces the risk of delays and errors. Alerts remain in the system, protecting patients from being exposed to allergens for their current and future admissions in HNELHD facilities.
For lower risk, unusual allergies and food intolerances, the project developed an interactive Food Allergy Tool. This resource is the first of its kind in NSW, and was developed to support clinicians in ordering the least restrictive menu option for their patient that is free from known allergens or intolerances. The Food Allergy Tool also guides clinicians in how to engage with patients to determine how to best manage their allergen, empowering the patient in their care. The Food Allergy Tool contains example meal plans and information on over 170 allergen and intolerances.

This alerts system and Food Allergy Tool have been successfully implemented in all overnight facilities across the District. The Food Allergy Tool has had excellent engagement, with over 170 visits per week to the website. In addition, over 800 staff completed an optional Food Allergy Management Education Module.
The rate of food allergies being entered into patients’ electronic record more than doubled in the first three months after launch. Most alerts (70%) are now entered directly by clinicians rather than by administration staff, and auditing has confirmed that the accuracy has also increased as expected.
Safer Baby Bundle - Working Together to Reduce Stillbirth
Safer Baby Bundle - Working Together to Reduce Stillbirth
 Stillbirth is a tragedy for the families involved and a serious public health problem with far reaching social, emotional and financial burdens on all involved. For every 1000 babies born in Australia, six will be stillborn. In many cases stillbirth is preventable, and research has found that 20-30% of late gestation stillbirths could be avoided with different care.
Stillbirth is a tragedy for the families involved and a serious public health problem with far reaching social, emotional and financial burdens on all involved. For every 1000 babies born in Australia, six will be stillborn. In many cases stillbirth is preventable, and research has found that 20-30% of late gestation stillbirths could be avoided with different care.
HNELHD is one of four health districts in NSW that are involved in the research phase of a national initiative to reduce the number of stillborn babies. The Safer Baby Bundle, as the name suggests, is a bundle of five interventions that reduce the risk of stillbirth. Each of these elements is evidence-based and emphasises the importance of best practice maternity care. HNELHD is committed to successfully implementing all five elements across all maternity services within the District.





Virtual Pharmacy Model – Improving Medication Safety in Mental Health Units
Virtual Pharmacy Model – Improving Medication Safety in Mental Health Units
In hospitals, clinical pharmacists work as part of the healthcare team to ensure patients are prescribed the most appropriate medications, provide education to patients and staff, and minimise the risk of medication-related harm. Patients admitted to hospital for treatment of mental illness often have complex medication arrangements. When treatment involves changes to medications, the risk of medication-related harm is increased.
HNE Mental Health Service has multiple acute inpatient facilities. The primary facility is the Mater Mental Health Hospital, located in Newcastle. Three smaller regional units at Maitland, Taree and Tamworth do not have regular access to specialised mental health pharmacist services locally.
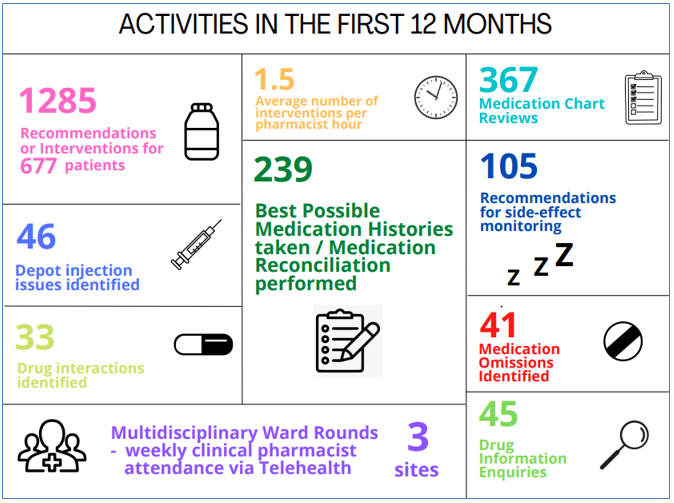
To address this challenge, the Mental Health Virtual Clinical Pharmacy Service was commenced as a pilot in July 2021. In this project, specialised mental health pharmacists at the Mater Mental Health Hospital took part in ward rounds at each of the three regional mental health units via telehealth. In addition to participating in ward rounds, the pharmacists conducted reviews of medication charts, collected medication histories, provided medication information and advice for patients, answered drug information enquiries and assisted with discharge medication planning.
The part-time service has proven to be highly effective. A staff survey has been conducted at participating facilities to evaluate the initiative. Results indicate that 70% of respondents found the telehealth service convenient, and 92% of respondents would like to see the service continued. The most frequently identified benefits of the service related to patient medication reviews, drug information, and support for discharge planning. In addition, three quarters of respondents reported that their knowledge of medications had improved since commencement of the project.
“I believe this service is extremely valuable for the care of our consumers. It enables us to ensure that the gold standard and evidence based medication is being prescribed during admission and that discharge medication issues are considered and resolved prior to discharge ensuring the best possible outcome for our consumers returning home.” - Survey respondent
The Virtual Clinical Pharmacy Project has enabled inpatient services in rural and regional parts of HNELHD to access specialised mental health pharmacy services. This initiative was presented at the CEC Virtual Clinical Roadshow, highlighting the scalability and cost-effectiveness of the service.
Improving the Patient Experience
Achieving the District’s vision of healthy people now and in the future can only be accomplished in partnership with the people we serve – patients, clients, their families, carers and our wider communities. Consumer representatives are valued members of committees, project teams and advisory groups at many different levels of the organisation.
The District Partnering with Consumers Committee is responsible for implementing tools and resources that support consumer engagement. These include Patient-Reported Experience and Outcome Measures (PREMs and PROMs), and the Health Literacy Ambassador Program.
Yarning up After Stroke - Engaging with community to co-design solutions
Yarning up After Stroke - Engaging with community to co-design solutions
The Yarning Up After Stroke (YuAS) project is a collaboration between the Aboriginal communities of the Tamworth Region, HNELHD’s Aboriginal Health Unit and Hunter Stroke Service, and research partners from University of Newcastle and University of New England.

We are also partnering with services based in community, The Tamworth Aboriginal Medical Service, building relationships with Walhallow Aboriginal Corporation Clinical Services and in continual talks with non-government services based in community that specialise in supporting Aboriginal people to live well after stroke.
The YuAS project supports Aboriginal communities, and those with lived experience of stroke within these communities, to identify solutions to challenges in accessing support and services following stroke. The project takes the approach of ‘yarning,’ which is a culturally respectful conversational way to share information, listen and learn. In Aboriginal culture Yarning Circles are safe spaces in which everyone can have a say.
The project was launched in Tamworth in May 2021, with Uncle Neville Sampson providing the Welcome to Country. People attended both in person and via Zoom from community and health services both within HNELHD and beyond. The team have conducted a number of individual yarn ups via Zoom and in person. A community yarn was held in March 2022 in Tamworth, and further group yarn ups are planned in the future with community members and with service providers who provide services to Aboriginal people living with stroke.
A family fun day was held in May 2022 at the Coledale Community Centre. The focus of the day was community engagement and sharing. Elders had the opportunity to share their own stroke journeys and the community enjoyed entertainment from celebrated local blues artist Buddy Knox and his family, and football star Nathan Blacklock came along to provided footy fun with the kids.
The YuAS team are developing a booklet to be used during yarning to help people living with stroke identify what is important to them, their goals and how they might achieve these goals. The tool is being co-designed with community and those with lived stroke experience, and feedback is being sought from services in community about other issues to consider in the stroke recovery journey.
Comprehensive Care - Consumer involvement improving what we do
The National Safety and Quality Health Care Standards highlights the importance of partnering with our consumers at many levels. This includes involving consumers as members of quality improvement teams to improve care.
A project has been occurring looking at how we can improve our risk screening processes on admission, as well as care planning that engages the whole Multi-Disciplinary Team as well as the patient, carer and family.
We have a very active consumer, Bill, who is a key member of the comprehensive care best practice project team. He has been involved in the development, trialling and evaluation of the documents we have developed. An example of Bill’s engagement was in developing a consumer rounding tool to be able to see if patients understand care planning and other aspects of care. He tested this rounding tool by carrying out the rounding himself on 2 wards at John Hunter Hospital. The results have informed next steps in the project. Members of the project team value Bill's contributions:
“This has been my first experience having true consumer rep, for me this has been a reflective and essential learning to ensure we put the consumer at the centre of everything we do.”
“Without Bill’s common sense approach keeping clinicians on track, I don’t think we would have developed the quality of product we have.”
“Having a consumer has challenged us to think outside of our own lane, ensure common language is used and to stay patient focused and patient centred.”
Bill himself enjoys the challenge of being part of the team:

A Workplace Culture that Drives Safe and Quality Care
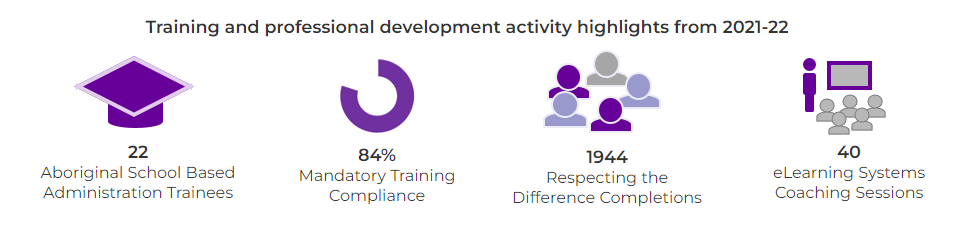
Hunter New England Local Health District supports many culture and capability building initiatives that foster safe and high-quality care. The HNELHD Applied Safety & Quality Program is a new program sponsored by the Clinical Excellence Commission that replaces previous clinical leadership programs.
The locally delivered 12-month program is currently being trialled with a cohort of 8 staff who will contribute to the evaluation of the program and become part of the future teaching faculty, ensuring sustainability into the future. This year’s projects cover a wide range clinical areas and topics, ranging from increasing availability of Respecting the Difference cultural respect training, supporting Morbidity and Mortality Meetings, and increasing the rate of spirometry assessments in rural facilities
John Hunter and Belmont Hospital Physiotherapy - Promoting Safety and Excellence
John Hunter and Belmont Hospital Physiotherapy - Promoting Safety and Excellence
The John Hunter and Belmont District Hospital Physiotherapy Department has realigned services to improve patient outcomes and enhance staff development opportunities, resulting in improved staff satisfaction. The team’s achievements cover a broad range of areas and reflect the sustained efforts of the team over the past several years.
Expanding practice to reduce surgical clinics wait times

Physiotherapy initiated advanced practice models of care in orthopaedics, neurosurgery, emergency, and maternity & gynaecology. Physiotherapists with specialised skills in these areas provide services with expanded scope, reducing the demand on clinics provided by medical and surgical teams. This in turn reduces the length of time patients need to wait to attend specialist outpatient services. Some of the new clinics set up include:
The Soft Tissue Injury clinic has reduced the demand on orthopaedic outpatient services. The proportion of patients presenting to emergency with soft tissue injuries who are referred to the Orthopaedic clinic has been reduced by 7%.
The Parallel Spinal clinic has enabled a reduction in waiting times for the Orthopaedic/Neurosurgical clinic. Patients were waiting up to two and a half years to attend surgical clinics, waiting times are now down to clinically recommended wait times.
The Shoulder Clinic has led to a 33% increase in capacity for new referrals to the surgical teams for assessment.
The advanced practice models have been built into published competency packages that have been used across the District and in other NSW health districts. The packages support and guide the professional development of junior physiotherapists as they expand their skill base.
Secondments supporting staff development and rural facilities
Rural facilities across the state face constant staffing challenges. The John Hunter and Belmont Physiotherapy team have implemented a rural secondment program that enables staff to gain experience in rural settings and provide rural facilities with much needed staffing support. So far 11 facilities have participated in the program, and staff development is supported by a rural practice competency and training package that has been implemented across the District.
Improvements in staff satisfaction has been demonstrated through the department’s results in the People Matter Employee Survey, with 100% of staff participating and improvements in every category in the most recent round of the survey. The team’s achievements resulted in them taking out the 2021 NSW Health People and Culture Award.

